Last month, Leon Schurgers. Ph.D., discussed with us why vitamin K2 was essential for bone health. To the surprise of many, studies continue to show that vitamin K2 is also essential for healthy arteries. Even Time magazine is now reporting that calcified arteries are a major risk factor in heart disease. What is the connection? Let’s discuss it with Dr. Schurgers.
Dr. Schurgers is a senior scientist in biochemistry at Maastricht University in the Netherlands. As a senior scientist for the division on vitamin K research, Dr. Schurgers is part of the Cardiovascular Research Institute, the largest research institute of the University of Maastricht. Dr. Schurgers’s major occupation is leading the scientific part on vitamin K research and supervising technical engineers, post-docs and Ph.D. students. Dr. Schurgers is a member of the American Society of Bone and Mineral Research, the International Society on Thrombosis and Haemostasis as well as the American Heart Association. He has published over 120 research papers in the international scientific press.
Passwater: Dr. Schurgers, we were discussing the role of vitamin K2, calcium and bone health last month. Let’s continue our discussion and consider the overall picture of vitamin K2, calcium and vitamin D. What happens when calcium intake is increased, but there is little vitamin D to help absorb it?
Schurgers: Calcium is needed for the heart, muscles and nerves to  function properly and for blood to clot. Inadequate calcium significantly contributes to the development of osteoporosis. Many published studies show that low calcium intake throughout life is associated with low bone mass and high fracture rate. National nutrition surveys have shown that most people are not getting the calcium they need to grow and maintain healthy bones.
function properly and for blood to clot. Inadequate calcium significantly contributes to the development of osteoporosis. Many published studies show that low calcium intake throughout life is associated with low bone mass and high fracture rate. National nutrition surveys have shown that most people are not getting the calcium they need to grow and maintain healthy bones.
However, when you increase the intake of calcium without the adequate amount of vitamin D, calcium’s health benefits cannot be achieved.
The body needs vitamin D to absorb calcium. Without enough vitamin D, one can’t form enough of the hormone calcitriol (known as the “active vitamin D”). This, in turn, leads to insufficient calcium absorption from the diet. In this situation, the body must take calcium from its stores in the skeleton, which weakens existing bone and prevents the formation of strong, new bone.
Passwater: What happens when calcium absorption is increased with vitamin D, but not much vitamin K is available to form active osteocalcin? Are there studies that indicate a risk?
Schurgers: During remodeling (i.e., the multi-step, dynamic process that replaces mature bone with new bone), the body releases calcium into the bloodstream to meet its metabolic needs, allowing the bone to change its size and shape as it grows or repairs from smaller injuries. As we emphasized in Part 1, bone is not static, inert or dead tissue. In healthy adults, remodeling rebuilds about 10% of the skeleton per year. Two types of cells regulate remodeling: osteoblasts build up the skeleton, while osteoclasts break it down. As long as the two cells are in balance, a healthy bone structure is maintained.
Osteoblasts also produce osteocalcin, which helps take calcium from the blood and bind it to the bone matrix. Osteocalcin influences bone mineralization, in part through its ability to bind to the mineral component of bone, hydroxyapatite, which in turn makes the skeleton stronger and less susceptible to fracture.
Here’s the kicker: Newly made osteocalcin is inactive. It needs vitamin K to become fully activated in order to bind calcium. This asset alone would make vitamin K2 a major player in the bone health category, but there’s also this: Vitamin K2 is transported adequately to bones, and helps deposit calcium into bones. Meanwhile, in the arteries, the vitamin K-dependent protein, matrix Gla protein (MGP), inhibits potentially fatal calcium accumulation in arteries. So, not only does vitamin K2 help with bone health, it plays a major role in managing cardiovascular health (CVH).
Passwater: Let’s discuss MGP, vitamin K2 and arteries in more detail later. Are there other studies about how vitamin K works with other nutrients for bone health?
Schurgers: Studies support the effectiveness of the collaboration between the vitamins. A study from Keio University revealed that vitamin K2 and vitamin D3 (cholecalciferol) “may be effective for mild postmenopausal osteoporosis.” In a 2010 article examining vitamins K and D published in The Alternative Medicine Review, Parris M. Kidd, Ph.D., verified their roles in bone health, CVH, and inflammation. He wrote that both vitamins K2 and D3 “can mutually enhance each other’s metabolism, a biochemical reciprocity consistent with clinical synergy.”
Passwater: So, vitamin K2 helps put calcium in the bones where it is needed. However, as you noted, there is even more to consider: healthy arteries. The March 10, 2014 issue of Time reported that screening arteries for calcium could get millions of people off statins. In the article, reporter Alice Park leads off with, “When it comes to predicting heart trouble, doctors essentially play a guessing game. So among all the factors they consider—such as a person’s age, weight, family medical history and cholesterol levels—it turns out that one of the most important reliable indicators may also be a bit unexpected: calcium.”
The Time article makes several points, including:
• 35% of people who have calcium buildup in their arteries—but no other heart disease risk factors—are almost four times as likely to have a heart event in seven years, compared with those who have zero calcium and some risk factors.
• Calcium can find its way into blood vessel walls. Once there, calcium attracts immune cells and forms dangerous plaques that stiffen arteries and generate clots that block blood flow to the heart, even causing heart attacks.
• More doctors are adding calcium screening to their tests to determine who really needs medication. If they see no calcium, they try to get patients off medicines.
Schurgers: There is a relationship between insufficient levels of vitamin K2 and the calcification of arteries. High tissue levels of vitamin K2 prevented the harmful calcification of arteries whereas low tissue levels of vitamin K2 enhanced calcification. The levels of vitamin K1 were essentially insignificant in both because vitamin K1 is only poorly taken into arterial tissue.
Passwater: Okay, arterial calcification—what we used to call hardening of the arteries—is a major risk factor for heart disease. How does calcium get into the artery wall and lining?
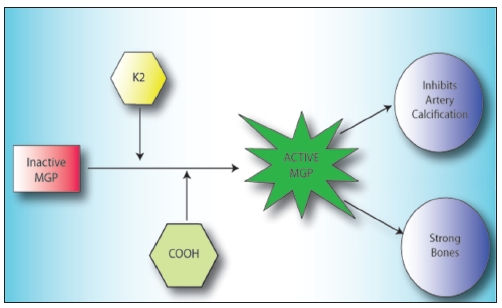
Schurgers: In circulation, vitamin K2 participates in adding a carboxyl group (COOH) to matrix Gla protein (MGP) which activates it. MGP is the most potent inhibitor of arterial calcification known, lowering the risk of vascular damage. MGP can be measured in blood, but exerts its effect in tissues where it binds calcium, preventing it from depositing in the vessel walls. In collaboration with other soluble factors and cells, MGP thus helps remove calcium from the arteries and keeps them elastic and flexible.
To properly perform its inhibitory function, MGP must be activated by vitamin K during the carboxylation process (see Figure 2). Vitamin K is needed to add the carboxyl group (COOH) to MGP. There are plenty of carboxyl groups available for this purpose, but there is usually inadequate vitamin K2 to fully carboxylate the MGP and make it active for calcium removal from the arteries. Vitamin K2 deficiency results in under-carboxylation of MGP and impairs their biological function. Without adequate vitamin K2 in the vessel walls, un-carboxylated MGP accumulates at the sites of calcium deposition and cannot inhibit calcification because it is inert. This, in turn, increases the risk of fatal cardiovascular events.
Adequate intake of vitamin K has been shown to lower the risk of vascular damage because it activates MGP, which inhibits calcium from depositing in the vessel walls (i.e., arterial calcification). When arteries become stiff from this process, it’s as though cement was poured in them, hardening the walls, which can impede healthy blood flow.
Inadequate vitamin K levels result in inadequate MGP activation, which greatly impairs the prevention of calcium inhibition and increases the risk of blood vessel calcification. Since this process occurs in the vessel wall, it leads to the wall stiffening of the vascular media and thickening via calcified plaques (typical atherosclerosis progression), which is associated with higher risk of cardiovascular events (see Figure 3).
|
| Figure 2: Vitamin K2 is needed to activate matrix Gla protein (MGP), which helps form healthy bones and inhibit arterial calcification. MGP is formed in bone cells and vascular cells in an inactive form. It must be activated through a process called carboxylation, which adds a carboxyl group (COOH) to MGP. Biochemically speaking, an enzyme adds a carboxyl group to form gamma-carboxyglutamic acid on a small number of vitamin K-dependent proteins. Carboxylation changes the calcium-binding properties of those proteins; this ability to bind calcium ions activates the proteins. There are three vitamin-K proteins in bone: MGP, osteocalcin (Gla protein) and protein S. MGP is also found in blood vessels, heart, lung and kidneys. The inactive form of MGP is called uncarboxylated MGP (ucMGP). |
|
|
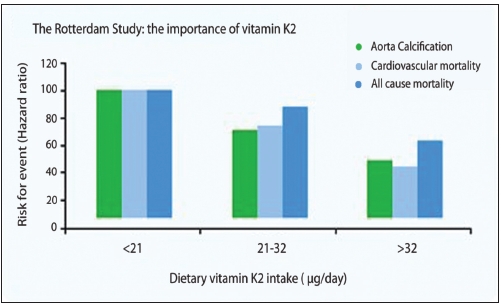
Figure 3: High vitamin K2 intake significantly promotes cardiovascular health (Geleijense et al., J. Nutr. 2004). |
Passwater: We discussed the Calcium Paradox in Part One and also in our earlier chat in 2009. The Calcium Paradox is where there is too little calcium in the bones and yet excess calcium accumulates in the arteries, making them stiff and inelastic. It’s five years later, so let’s bring our readers up to date. What were the early clues that vitamin K2 could help keep calcium out of artery walls where it is harmful?
Schurgers: In kidney dialysis patients, the high calcium and phosphate concentration (due to impaired kidney function) results in artery calcification—especially when dialysis patients turn out to be vitamin K deficient! The same holds true for the apparently healthy population, in which excessive calcium is released by bone loss and by high intake of calcium supplements. When this is not regulated and controlled in the body, vascular calcification is initiated. Also here, it is likely that a vitamin K deficiency is accelerating the process of vascular calcification.
Passwater: Is this strictly a theoretical problem or are there actual clinical studies linking high dietary and/or supplemental calcium—or the lack of adequate vitamin K2—with cardiovascular disease?
Schurgers: There are actually numerous studies, summarized in meta-analysis, clearly indicating such a link between calcium intake and cardiovascular disease. But when you think about the theory of it all, one cannot discount how absolutely sensible it is.
The population-based Rotterdam study evaluated 4,807 healthy men and women over age 55 and the relationship between dietary intake of vitamin K and aortic calcification, heart disease and all-cause mortality. The study revealed that high dietary intake of vitamin K2 (at least 32 mcg per day) and not vitamin K1, reduced arterial calcification by 50%, cardiovascular death by 50%, and all-cause mortality by 25% (see Figure 3).
These findings were supported by another population-based study published in 2009 with 16,000 healthy women (aged 49-70) from the Prospect-EPIC cohort population. After eight years, the data showed that high intake of natural vitamin K2, but not vitamin K1, helps protect against cardiovascular events; for every 10 mcg of vitamin K2 consumed, the risk of coronary heart disease was reduced.
In still another study, 244 post-menopausal women supplemented with 180 mcg of vitamin K2 as MK-7 actually showed a significant improvement in cardiovascular health as measured by ultrasound and pulse-wave velocity, which are recognized standard measurements for cardiovascular health. In this trial, carotid artery distensibility (i.e., elasticity, or the ability for a blood vessel to stretch or dilate) was significantly improved over a three-year period as compared to the placebo group. Also, pulse-wave velocity was significantly decreased in the vitamin K2 (MK-7) group, but not the placebo group, demonstrating an increase in the elasticity and reduction in age-related arterial stiffening.
A study on 564 post-menopausal women also revealed that vitamin K2 intake decreases coronary calcification, whereas vitamin K1 does not.
In a recent study published in the American Journal of Kidney Disease, researchers examined 53 long-term hemodialysis patients in stable conditions, who were supplemented with menaquinone-7 (vitamin K2) at varying levels of 45, 135 or 360 mcg/d for six weeks; 50 healthy age-matched individuals served as controls. The efficacy of vitamin K2 treatment was assessed by measuring ucMGP.
These results confirmed that most dialysis patients have a vitamin K deficiency and that vitamin K2 supplementation promoted a dose- and time-dependent decrease of ucMGP, uncarboxylated osteocalcin and uncarboxylated prothrombin. The best efficacy was seen with the highest dose of vitamin K2 (360 mcg/d), where a 93% reduction in inactive MGP levels was shown.
The aim of this study was to investigate whether daily vitamin K supplementation (MK-7) improves the bioactivity of vitamin K-dependent proteins in hemodialysis patients. Indeed, this study clearly showed evidence of a functional vitamin K deficiency in hemodialysis patients, and that it can be treated effectively by vitamin K2 (MK-7) supplementation.
Passwater: What was the dosage used in the studies?
Schurgers: The dose used for the three-year study showing bone and  heart benefits was 180 mcg per day. This is what we recommend, for now, as it is the dose that was responsible for the improvements.
heart benefits was 180 mcg per day. This is what we recommend, for now, as it is the dose that was responsible for the improvements.
Passwater: These studies certainly demonstrate that vitamin K2 is critical for both bone and artery health, but there is more for us to discuss. Let’s chat more about vitamin K2 in the next column and take a brief look at new research on memory and longevity. WF
Dr. Richard Passwater is the author of more than 45 books and 500 articles on nutrition. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com.
Published in WholeFoods Magazine, July 2014










