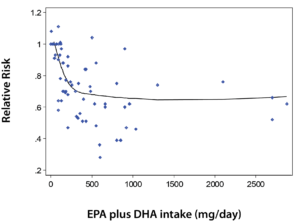
The researchers concluded, “Our comprehensive meta-analysis of data from RCTs and prospective cohort studies supports this recommendation. Although not statistically significant, a 6% reduced risk of any CHD event was observed among RCTs, a finding supported by a statistically significant 18% reduced risk of CHD among the prospective cohort studies. From a clinical perspective, our results indicate that EPA+DHA may be associated with reducing CHD risk to a greater extent in populations with elevated triglyceride levels or LDL cholesterol, which are risk factors that impact a significant portion of the general adult population in the United States.”
In 2012, I had the honor and privilege of co-authoring “The Missing Wellness Factors – EPA and DHA” with Professor Jørn Dyerberg, M.D., DMSc., the discoverer of the vital health benefits of fish oil EPA and DHA (2). Dr. Jørn Dyerberg went on five expeditions to the remote Greenland Inuits in the Arctic Circle. As we stated in Chapter Six, “(T)he take-home message of this book is that adequate amounts of the omega-3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are needed for optimal health. Unfortunately, through the past fifty years, the amounts of EPA and DHA have decreased considerably and at an ever-increasing pace.”
Last year, an interesting study confirmed that many people worldwide may not be getting optimal levels of the EPA and DHA (3). Professor Manfred Eggersdorfer, whom we have chatted with in this column before, was close to that study and is familiar with the study and its implications.
Dr. Eggersdorfer is a professor of healthy ageing at the University Medical Center Groningen (UMCG) in the Netherlands and the senior vice president of DSM Nutritional Products, in Basel, Switzerland. He studied chemistry at the Technical University Munich and earned his Ph.D. in organic chemistry in the field of synthesis and characterization of unusual amino acids. He completed his post-doc at the Stanford-University, California, working with Carl Djerassi on the isolation and characterization of sterols from marine origin as potential contraceptives. He joined Roche, Basel, Switzerland in 1999 as head of research and development of vitamins and continued in this role after Roche was acquired by DSM in 2003.
Dr. Eggersdorfer holds the chair for Healthy Ageing at the UMCG and is responsible for nutrition science and advocacy at DSM Nutritional Products. His scientific work focuses on the role of essential nutrients for health, vitality and well-being, especially on the impact of inadequate intake and status of micronutrients on long term health and healthy ageing. He is active as an advisory board member at the Johns Hopkins Bloomberg School of Public Health, of the Strategy Board of the Institute of Food Science University Hamburg, and affiliate of various other organizations. He is the author of numerous publications in the fields of vitamins, innovation in nutritional ingredients and a scientific reviewer for a variety of journals.
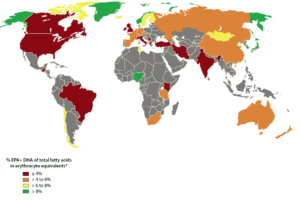
Passwater:The study I mentioned examined the data included in nearly 300 previous studies and grouped the levels of EPA and DHA into four categories. They then prepared a global map which graphically shows the results. What were the findings?
Eggersdorfer: Omega-3s are essential poly-unsaturated long chain fatty acids. Humans are unable to synthesize them and so they must be provided by the diet. The most important omega-3 poly-unsaturated acids for humans are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). It is reported that omega-3 intake via the diet and/or supplements is very low in many countries. This paper is the first of its kind to summarize not the intake of omega-3s but blood levels. Reporting blood levels is more accurate and informative because it eliminates potential issues with under- and over-reporting and takes care of bio-availability, personal set up and other factors. In this paper the scientists define four ranges to assess the status of omega-3s: blood levels below 4% EPA plus DHA as very low, blood levels of 4 to 6% as low, 6 to 8% as insufficient and above 8% as optimal. In the medical community, the ranges used in the paper are also established as reference values for omega-3s.
According to this paper, blood levels of EPA and DHA vary across the globe, with most of the countries and regions of the world having levels that are considered as low to very low. The very low to low range of blood EPA and DHA may have implications for the individual as well as for the society because of higher risks for non-communicable diseases (also called chronic diseases), in particular cardiovascular diseases and cognitive decline. The paper summarizes data from 54 countries—more data on blood levels of EPA and DHA are needed because for large regions of the globe, particularly for developing countries, data are missing. A recent meta-analysis, to date the most comprehensive quantitative analysis of its kind within the peer reviewed biomedical literature, showed a significant decrease of CHD risk in people with elevated triglyceride (TG) and LDL-cholesterol levels (1).
Passwater:The researchers concluded that many people are in the very low to low range of blood levels of EPA and DHA which increases global risk for chronic disease. This is a serious statement. What exactly are the researchers trying to tell us?
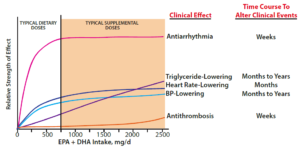
Eggersdorfer: As said, omega-3 poly-unsaturated acids are essential for humans and they have to come via the diet or supplements. Very low intakes are associated with deficiency symptoms, which include impaired barrier function and wound healing, failure to thrive, and poor neurological and visual development in infants. For adults EPA and DHA contribute to risk reduction for coronary heart disease, risk reduction for cognitive decline and all-cause dementia and possibly other chronic, degenerative diseases. The effect of both EPA and DHA on lowering triglyceride (TG) levels is well established and is the basis as a prescription medication for people with hypertriglycidemia. Optimal omega-3 levels are associated with a reduced risk of coronary heart disease with the major proposed mechanism of a reduction in fatal arrhythmias, TG lowering, heart rate lowering and blood pressure lowering. Please see figure 2.
The role of omega-3s seems to be appreciated in regions with a higher omega-3 intake and status, such as Scandinavia and the Sea of Japan, as people in these regions tend to consume a larger amount of fish than other regions. People in the regions with the higher omega-3 status may also have a greater understanding of the benefits of supplementation. The regions with low omega-3 levels are widespread — particularly in the Western World. This may not only reflect their dietary habits, but also the consumer hesitant attitudes towards the use of supplements.
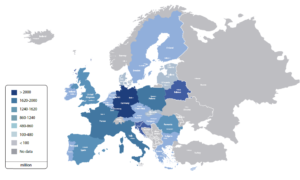
Source: Frost & Sullivan 2016
The impact of an optimal omega-3 status on the reduction of cardiovascular events and the related savings in health care costs was recently evaluated for the European Union and identified a potential saving of EUR 12.9 billion per year assuming a 4.9% reduction of cardiovascular events. Please see figure 3.
Passwater:In our book, Professor Dyerberg and I call for the establishing RDA for both EPA and DHA. Several others, including William Harris, who was kind enough to write our foreword and has chatted with us in this column, have also called for EPA and DHA RDAs. Does this study have any relevance for the need to establish dietary recommendations for EPA and DHA?
Eggersdorfer: This review is the first of its kind to show that blood levels of EPA and DHA across the world are considered low to very low. We believe there is a strong case for health authorities to issue recommendations relating to omega-3 and a reduction in the risk of experiencing cardiovascular disease (CVD) events and cognitive decline, alongside other recommendations in this area, such as a healthy diet and increased physical activity.
The recommended daily intake of omega-3 is variable and depends on the individual health profile, blood pressure levels, blood TG levels, and other health parameters. This has made it difficult for regulators to set a standard intake level. However, there is a proposed adequate daily intake of 250 to 500 mg for EPA and DHA for all adults for normal health and wellness.
The typical amount level found in a single 1,000 mg non-concentrated omega-3 fish oil capsule is 250 mg to 300 mg of EPA and DHA. On the other hand, European Food and Safety Authority (EFSA) has investigated the quantity of EPA and DHA required for specific health benefits in the context of assessments of applications for health claims authorisations. These opinions indicate that an intake of 2 g of EPA/DHA is required for the maintenance of normal blood TG levels and 3 g for the maintenance of normal blood pressure.
The findings of this paper are a stimulus to academia for more research in the field of omega-3s, and to health authorities and health care professionals to dedicate more attention to the intake, status and role of EPA and DHA in human health and in health care systems.
Passwater:Dr. Dyerberg and myself suggest in our book that a total daily intake of 1,000 mg per day or more of EPA plus DHA would improve health and help protect against many chronic diseases. Does this new study offer any suggestions about desirable intakes of EPA and DHA? What are your recommendations?
Eggersdorfer: This suggestion is very much in line with the findings and recommendation by EFSA. To achieve cardiovascular benefits, it seems to be necessary to have an intake of omega-3s that is significantly above the level of 250 – 500mg per day in order to reach the >8% level (shown on the map in green) for the omega-3 status. In this paper, the authors argue that a minimum intake of 1 g per day would be necessary to achieve the 8% level (even more, in some individuals).
A meta-analysis by Drs. D. Mozaffarian and Eric Rimm of the Harvard Medical School of 16 prospective cohort studies and four randomized controlled trials including 326,527 subjects from the US, Europe and Asia found a total risk reduction of 36% for cardiac death using doses of 500 mg/day or more. Back in 1995, a paper by Siscovic et al. in the journal JAMA even indicated that raising the intake level from 70 mg to 1000 mg in the USA would reduce the risk of cardiac death by 90% (5)!
Low levels of omega-3s are also associated with higher risk for Alzheimer’s disease, other types of dementia and cognitive impairment. On mental health, Captain Joe Hibbeln of NIH and others say 1 g a day of EPA and DHA are needed for good psychological health. A recent meta-analysis on depression says that marine omega-3s are only effective if the amount of EPA is greater than the DHA.
Food supplements and fortified foods are a convenient way to ensure that the optimal level can be achieved. This review indeed adds to recent research which indicates that adequate omega-3 intake has beneficial effects on the risk reduction of cardiovascular disease and cognitive decline associated with normal ageing.
Passwater:The benefits most often cited for optimal intakes of EPA and DHA include cardiovascular and neurological benefits. Why are EPA and DHA so important here?
Eggersdorfer: Omega-3 poly-unsaturated fatty acids have a number of health effects next to the mentioned benefit in lowering TG levels and reducing hypertension, like reducing platelet aggregation and especially acting anti-inflammatory. Where inflammation is uncontrolled or excessive or continues unabated, tissue damage and metabolic changes occur. Omega-3 fatty acids exert anti-inflammatory effects by inhibiting production of arachidonic acid-derived eicosanoids. Omega-3 fatty acids are readily incorporated into inflammatory cells and alter cell signalling, gene expression and production of eicosanoids and resolvins.
Omega-3 fatty acids can counter the effects of classic inflammatory stimuli like lipopolysaccarides and of saturated fatty acids, the mechanistic evidence for this is excellent. They may have a role in controlling inflammation in people with frank inflammatory conditions. So in summary, long term exposure to omega-3 fatty acids may impede the development of chronic low grade inflammation which is associated with cardio-metabolic diseases. Please see figure 5.
In this context, let me mention a study performed this year by Dr. S. Greene et al. replicating the famous 1999 GISSI study (7). This new study in Italy demonstrated that omega-3s have an additional benefit in patients, which had a heart attack event, even when the patients took pharma drugs as therapies. Dr. Greene argues that the new, large cohort study clearly demonstrates that an intervention of 1 g per day of marine omega-3 fatty acids in patients who had recently suffered a myocardial infarction (MI) produces a substantial benefit next to the pharmaceutical drug.
Passwater: You mentioned inflammation as a risk factor for cardiovascular health. Most of the public is still focusing on cholesterol as the primary risk factor, whereas most of the researchers in the cardiovascular field have moved on to inflammation as the major risk factor. How is inflammation involved in heart disease?
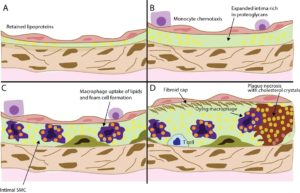
Eggersdorfer: It is true, that cholesterol (actual oxidized high density LDL) is a risk factor for cardiovascular disease in people, but it is only one of many. Inflammation is linked to several diseases. For this reason, it gets a lot of attention in the medical community and in science. For example, the intima (blood vessel linings) seems to play an important role in CVD and enables the initiation of plaque formation. Omega-3s induce the production of a series of anti-inflammatory metabolites and by doing this reduce inflammation and the production of spick plaques.
Passwater:Isn’t vitamin E also very important in cardiovascular and neurological health, and acting as anti-inflammatory agent? Don’t EPA+DHA increase the need for antioxidants, such as vitamin E, and improved levels also require more vitamin E? What is your guidance for vitamin E intake and EPA+DHA intake together?
Eggersdorfer: Correct, vitamin E is for humans an essential micronutrient and lipid soluble antioxidant, preventing the spread of free-radical reactions. Vitamin E is located within the cellular membranes and protects the polyunsaturated fatty acids, mainly omega-3 fatty acids

EPA and DHA, from oxidation by free radicals. So the main function of vitamin E is to protect omega-3s from oxidative damage. A number of studies show that the vitamin E requirement is related to the dietary intake of omega-3s. Thus, to quantify the vitamin E requirements, a basal vitamin E intake plus an additional vitamin E requirement for dietary omega-3s is considered and recommended. The intake recommendation in some countries, for this reason, take into account the intake for omega-3s in the vitamin E recommendation. The precise vitamin E/PUFA ratio varies in individuals depending on types of diet and health status.
Recent research suggests that a vitamin E intake (as an adult 15 mg/day) combined with the additional requirements varied from 12 to 20 mg/day for a typical range of dietary PUFA intake has beneficial effects on the immune system, cognitive function, cardiovascular health on reducing the risk for infections.
Passwater:Thanks you Professor Eggersdorfer for helping explain that many people are not getting the optimal amounts of EPA and DHA.
References
- Dominik D. Alexander, D.D., Miller, P.E., Van Elswyk, M.E., et al. A Meta-Analysis of Randomized Controlled Trials and Prospective Cohort Studies of Eicosapentaenoic and Docosahexaenoic Long-Chain Omega-3 Fatty Acids and Coronary Heart Disease Risk. Mayo Clinic Proceedings 92:1;15 – 29 (Jan 2017).
- Dyerberg, Jørn and Passwater, R. The Missing Wellness Factors – EPA and DHA: The Most Important Nutrients Since Vitamins. Basic Health Publications, Inc., Laguna Beach, CA. (2012).
- Stark KD, Van Elswyk ME, Higgins MR, Weatherford CA and Salem N Jr. Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog Lipid Res. 2016 Jul;63:132-52. doi: 10.1016/j.plipres.2016.05.001.
- Mozaffarian D and Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006 Oct 18;296(15):1885-99.
- Siscovick DS, Raghunathan TE, King I, et al. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA. 1995 Nov 1;274(17):1363-7.
- Wong BW, Meredith A, Lin D, and McManus, BM. The Biological Role of Inflammation in Atherosclerosis. Canadian Journal Card. 28(6)631-641(2012).
- Greene SJ, Temporelli PL, Campia U et al., “Effects of Polyunsaturated Fatty Acid Treatment on Postdischarge Outcomes After Acute Myocardial Infarction”; Am J Cardiol. 2016; 117: 340–346.

Dr. Richard Passwater is the author of more than 45 books and 500 articles on nutrition. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com.










