Part Three of a Five-Part Series on Heart Health
It seems as if, for most of the medical community today, the question is not if a patient is suited for statin use, but “How soon can we get you on them?” It’s hardly hyperbole: According to statistics from the 2005–2008 government health survey, approximately 32 million Americans were taking a statin drug. This roughly equals the populations of Florida and Illinois combined.
But, the cholesterol statistics for those over the age of 45 are on a downward trend, which is the main intention of widespread statin use (1). This has meant, plainly and simply, a drop-off in serious cardiovascular incidents among those taking statins. This benefit is undeniable, but there is much more to the story. For one, statins don’t cover the entire spectrum of what we can do for our cardiovascular health, so perhaps we had better look to support these other areas, too. In addition, the stories, and the studies, keep piling up about the serious side effects statins produce in some individuals. It is definitely worth examining what these are, and how natural supplements may help lessen and prevent them.
Statins: Getting to Know You
 The primary goal of statin use is to lower cholesterol for the betterment of cardiovascular health. Other mechanisms of action, however, may also be beneficial. For our purposes, it will help first to know how statins achieve these ends, before we examine what they leave to be desired, and what some of the collateral damage might be.
The primary goal of statin use is to lower cholesterol for the betterment of cardiovascular health. Other mechanisms of action, however, may also be beneficial. For our purposes, it will help first to know how statins achieve these ends, before we examine what they leave to be desired, and what some of the collateral damage might be.
Another, more descriptive way to refer to statin pharmaceuticals is to call them HMG-CoA reductase inhibitors. “Statins inhibit the enzyme HMG-CoA reductase in the liver and other tissues including the vascular system,” says Mark Houston M.D., associate clinical professor of medicine at Vanderbilt University, and author of best-sellers including What Your Doctor May Not Tell You About Heart Disease and What Your Doctor May Not Tell You About Hypertension. He describes the role of HMG-CoA as the rate-limiting step in cholesterol production. HMG-CoA reductase inhibitors compete with the enzyme for space at this stage, thereby cutting down on the production of cholesterol later in the process.
Explaining the significance of reduced cholesterol at the molecular level is Kira Schmid, N.D., associate director of scientific affairs for Life Extension, Fort Lauderdale, FL. “Statins reduce the number of cholesterol particles interacting with the arterial wall, lessening the likelihood of plaque formation in the arteries,” she says.
There is a further mechanism of action that occurs when the HMG-CoA enzyme is inhibited in the liver, which involves the activation of receptors for bad cholesterol. “The enzyme is anchored in the membrane of the endoplasmic reticulum. Inhibitors of the enzyme initiate the expression of low density lipoprotein (LDL) receptors in the liver, which increases the breakdown of LDL cholesterol, lowers the level of cholesterol in the bloodstream and in doing so, reduces the rate of the atherosclerotic process,” says Jolie Root, LPN, LNC, nutritionist and educator for Carlson Laboratories, Inc., Arlington Heights, IL. Cholesterol levels are therefore decreased in more than one way.
 The action of statins, Houston says, also results in interference with several other pathways in a manner that benefits cardiovascular health. In doing so, it unfortunately may cause nutrient depletions and other side effects which we’ll get to later. Alteration of these downstream channels, called pleiotrophic pathways, may decrease inflammation, oxidative stress and immune function. It also improves endothelial health through nitric oxide production, reduces atherosclerosis and clotting risk and benefits blood pressure (2). On top of lowering LDL cholesterol, many of these actions are likely important in the reduction of cardiovascular disease, heart attack and stroke due to statin use.
The action of statins, Houston says, also results in interference with several other pathways in a manner that benefits cardiovascular health. In doing so, it unfortunately may cause nutrient depletions and other side effects which we’ll get to later. Alteration of these downstream channels, called pleiotrophic pathways, may decrease inflammation, oxidative stress and immune function. It also improves endothelial health through nitric oxide production, reduces atherosclerosis and clotting risk and benefits blood pressure (2). On top of lowering LDL cholesterol, many of these actions are likely important in the reduction of cardiovascular disease, heart attack and stroke due to statin use.
After acknowledging that statin use will lower cardiac risk in many individuals, another source cites yet another potential biochemical action underlying this effect. “This important benefit of statins is mediated by a mechanism that was not recognized until only recently—that of nuclear factor Kappa B (NFkB) inhibition,” says Duane Graveline, M.D., MPH, former NASA astronaut and author of www.spacedoc.com, as well as several books on statin drug side effects. He says that with statin use, two things happen at the same time: cholesterol-lowering effects that can lead to a host of side effects, and NFkB inhibition that leads to improved cardiovascular health.
Both the public, through a newly encouraged awareness of their cholesterol numbers, and the medical establishment, through convincing statistics about heart healthy benefits, were gradually introduced to statins by the pharmaceutical industry, and now their prescription is nearly a matter of routine. “They’ve become the drug of choice for the treatment of hypercholesterolemia, which is an established risk factor for cardiovascular disease,” says Robert Barry, Ph.D., executive director of scientific affairs for Kaneka North America, LLC, Pasadena, TX. Though their relative value as primary care (a preventive measure for healthy individuals) and secondary care (for those at high risk of or already dealing with cardiovascular issues) is up for debate, they are often used in both contexts.
Rounding out the Picture
There’s more to cardiovascular wellness than cholesterol reduction. Therefore, “Statins are not a ‘cure-all’ for cardiovascular disease; a comprehensive approach is required to effectively lower risk,” says Schmid. Other crucial factors can include cholesterol oxidation, hypertension, excess plasma glucose, being overweight, fibrinogen, homocysteine levels, vitamin K and vitamin D deficiencies and hormone imbalances.
Besides its oxidative status (more on that in a moment), the size and density of cholesterol particles can determine the level of cardiovascular risk an individual faces. According to Schmid, large, buoyant LDL particles are less dangerous than small, dense LDL particles. Conversely, larger HDL (good cholesterol) particles may offer greater vascular protection than smaller ones. “Statins do not adequately address small, dense LDL particles,” she says.
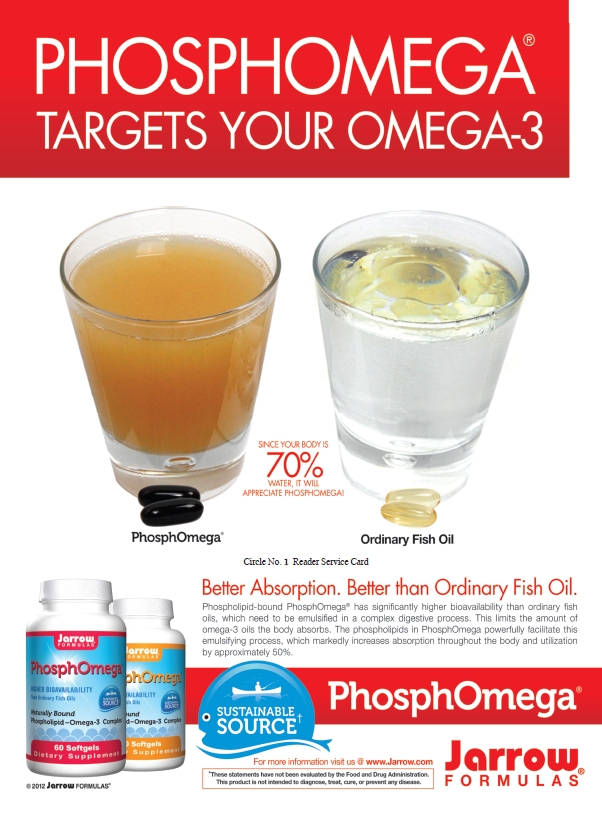
Omega-3 fatty acids and niacin have both  been shown to influence cholesterol particle size for the better. For cholesterol management in general, niacin, fiber, amla and theaflavins from black tea are all nutraceuticals that can help, according to Schmid.
been shown to influence cholesterol particle size for the better. For cholesterol management in general, niacin, fiber, amla and theaflavins from black tea are all nutraceuticals that can help, according to Schmid.
The Japan Eicosapentaenoic acid (EPA) Lipid Intervention Study (JELIS), according to Root, tested the effects of long-term EPA use at 1,800 mg/day, in addition to a statin, in patients with hypercholesterolemia (3). “The results add support to previous evidence of the beneficial effect of omega-3 fatty acids in patients with known coronary heart disease, and show that that effect can extend the benefit of statins,” she says.
Statins are known to fall short in other ways, too, including the fact that they do not affect other important biochemical markers for heart health. States Angelica S. Vrablic, Ph.D., manager of nutrition research for Solgar Vitamin and Herb, Leonia, NJ, “Statin pharmaceuticals are not known to have effects on other blood lipids, such as triglycerides.” Elevated levels of triglycerides are often correlated with insulin resistance and a high-carbohydrate diet, and as many consumers know, high levels of these fatty compounds in the blood can be bad news for cardiovascular health. Exercise, proper diet and increased omega-3 intake are common solutions to high triglycerides (4).
While statins may address some aspects of inflammation, the inflammatory cascade is a complicated process, and checking on inflammatory markers such as C-reactive protein can be key for high-risk individuals, according to Rob Maru, chief innovation officer for Reserveage Organics, Gainesville, FL. Statins may not address these issues fully, but potent antioxidants often can stem the tide of inflammation. His company does not view cholesterol itself as the threat, but instead urges a focus on oxidized LDL. “Antioxidants such as resveratrol slow that oxidation process,” Maru says.
For benefiting heart health in ways that statins usually do not, and for extending or complementing the positives of statin use, Houston lists and describes several other supplements. A few may also be of use in combating the side effects we’ll soon tackle. Keep in mind that any and all adjustments to diet or supplement routines should be made in cooperation with a doctor, particularly for those already on statins or other drugs. Likewise, no supplement should be construed as a substitute for or reason to adjust the dosage of a current prescription, without a discussion with a physician or specialist.
 Gamma and delta tocotrienols, specific components of the vitamin E class of compounds, are thought to interfere with HMG-CoA reductase, potentially adding an additional 10–15% reduction in LDL when combined with a statin, according to Houston. They may also increase the synthesis of coenzyme Q10 (CoQ10), improving ATP production and reducing oxidative stress. Gamma and delta tocopherols, different forms of vitamin E, may improve cell membrane function and improve oxidative stress and inflammation.
Gamma and delta tocotrienols, specific components of the vitamin E class of compounds, are thought to interfere with HMG-CoA reductase, potentially adding an additional 10–15% reduction in LDL when combined with a statin, according to Houston. They may also increase the synthesis of coenzyme Q10 (CoQ10), improving ATP production and reducing oxidative stress. Gamma and delta tocopherols, different forms of vitamin E, may improve cell membrane function and improve oxidative stress and inflammation.
As a cofactor in many reactions throughout the body, including immune and thyroid function, selenium is a good ally in the fight for heart health. Like others in this list, it can decrease oxidative stress and inflammation and improve muscle function.
Carnitine can help reduce the risk of congestive heart failure, according to Houston, while improving exercise performance and energy. Some of this benefit may come through improved cardiac and skeletal muscle function, an area that may suffer with statin use. Creatine and d-ribose are also means to support skeletal muscle. D-ribose, says Houston, is a five carbon sugar that can reduce fatigue and boost exercise efforts via ATP production, while benefiting angina and congestive heart risk.
Finally, the sunshine vitamin, vitamin D, in high concentrations can also be of use for cardiovascular health issues, since it is involved at the genetic level with many bodily processes.
Navigating Statin Use
Once an individual is placed on a statin, it is not always smooth sailing toward cardiovascular wellbeing. There are often slight, and less frequently, quite serious tradeoffs made on this journey. The people that are likely to suffer the worst due to these side effects, which range from muscle issues to memory loss, include the physically active and the elderly. Those that exercise often and at high intensity may see problems in recovery and performance with statin use, for instance.
For the advanced in age, any weakening of the muscular system can be ill-afforded, since muscle loss is likely already occurring as part of the aging process, Root points out. The cognitive problems that are now being associated with statin use may also hit the elderly harder. Root says that there are trials indicating a decline in cognitive function with statin use, as well as several case reports (5). Severe irritability may also become a problem in some individuals, according to Root.
In addition, those that are female, on high statin dosages, on lipid-soluble statins, have insulin resistance, have diabetes or metabolic syndrome, and that are obese may be predisposed to complications, according to Houston. Schmid adds that those with preexisting liver problems may not do well with statins.
The most high-profile drawback of statin use is their propensity to reduce CoQ10 levels, a fundamental piece of the body’s energy production puzzle. “When levels of CoQ10 are depleted, there is less energy available to the muscles. Statin use has been linked to muscle fatigue and pain which may surface as soreness and weakness,” explains Maru. This unfortunate side effect and the reason behind it could be viewed as somewhat ironic. The heart is the most energy-demanding organ in the body, Barry points out, and statins can deplete it of its energy source.
“This could be related to the fact that statins lower plasma LDL levels, and CoQ10 is mainly transported by LDL, but a decrease is also found in platelets and in lymphocytes of statin-treated patients, pointing to true inhibition of CoQ10 synthesis,” says Root. Trisha Sugarek MacDonald, B.S., M.S., director of R&D and national educator for Bluebonnet Nutrition Corporation, Sugar Land, TX, confirms that HMG-CoA reductase also underlies the synthesis of CoQ10, as well as dehydrocholesterol, a prohormone for vitamin D3. “Therefore, it would be proper to have these nutrients measured in the blood when evaluating cholesterol levels,” she says, adding that statin users could be considered candidates for supplementation in these and other areas.
CoQ10, in and of itself, is considered an important aid to cardiovascular health because of its role in energy production, as well as its powerful antioxidant properties. “You slow down synthesizing CoQ10 greatly by mid-life. You stop synthesizing it entirely when you are elderly. It is absolutely critical for function,” says Graveline. Barry notes that all of our metabolic functions, including those of our brain neurons, are fueled by ATP, and CoQ10 is required for ATP production. Significant for those facing memory issues tied to statin use are the early research findings that it is reversible. If statin use is stopped, any lost cognitive function seems to return, according to Barry. It is important to realize, however, that “CoQ10 supplements are not intended to serve as a replacement for statin therapy, nor should you discontinue taking any prescribed medications while supplementing with CoQ10,” cautions Vrablic.
Barry summarizes that while statins reduce cholesterol, they don’t do so selectively, and CoQ10 depletion is one example of this. CoQ10 is crucial for mitochondrial energy transport throughout the body, including in skeletal muscle. “The depletion of CoQ10 can induce mitochondrial dysfunction,” he says, and the end result of this includes reduced energy and aerobic capacity. It can also mean the development of myopathy symptoms like cramps, weakness, fatigue and pain. “Typically, if a patient exhibits myalgia with statin use, if they are taken off the statin and then put back on the statin, it comes back worse than it was before,” Barry says.
 There is a rare but recognized end result of this pattern of side effects to be considered. Says Root, “The most commonly discussed serious adverse effect of statins is rhabdomyolysis—a condition in which there is severe breakdown of muscle tissue that may be toxic to the kidneys and result in kidney failure or death,” adding, “Shortness of breath sometimes accompanies statin-associated muscle problems. Occasionally, shortness of breath is the predominant symptom.” There is also, according to Barry, the potential for ALS-like symptoms and other symptoms common to age-related neurodegenerative diseases.
There is a rare but recognized end result of this pattern of side effects to be considered. Says Root, “The most commonly discussed serious adverse effect of statins is rhabdomyolysis—a condition in which there is severe breakdown of muscle tissue that may be toxic to the kidneys and result in kidney failure or death,” adding, “Shortness of breath sometimes accompanies statin-associated muscle problems. Occasionally, shortness of breath is the predominant symptom.” There is also, according to Barry, the potential for ALS-like symptoms and other symptoms common to age-related neurodegenerative diseases.
A preliminary study (6) that Barry cites opened up the scientific line of inquiry into muscle pain as a side effect, and now the National Institutes of Health has funded several studies on CoQ10 supplementation coupled with statin use, which are taking place in major medical centers across the country. He thinks the increased visibility of these issues is due to the increased use of statins, especially in younger populations. Side effects like these can lead to substantial noncompliance and attempts by individuals to shift around statin dosages, Barry says.
The issues go well beyond the realm of muscles. “There are now numerous scientifically documented problems with statins that may mitigate their ability to reduce cardiovascular disease,” says Houston, listing heart failure, gastrointestinal symptoms, insomnia, pancreatic dysfunction and sexual dysfunction in addition to the problems already discussed.
There may also be a risk of exacerbating cases of diabetes. “Recently, it has been reported in the Canadian Journal of Cardiology that statin use has been associated with elevated levels of glycosylated hemoglobin and fasting glucose levels, which collectively increases the risk for diabetic complications,” says Sugarek MacDonald (7). Due to this potential hazard, some 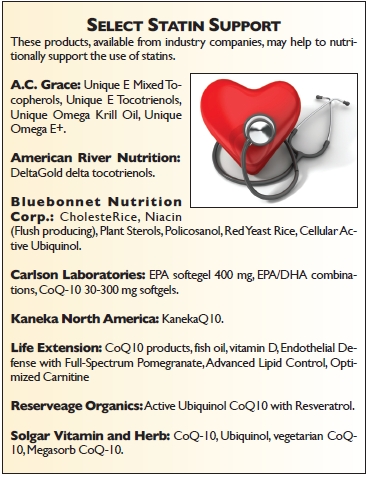 doctors may recommend a more natural approach for diabetics who would otherwise be prescribed a statin, consisting of exercise as well as diet and lifestyle changes.
doctors may recommend a more natural approach for diabetics who would otherwise be prescribed a statin, consisting of exercise as well as diet and lifestyle changes.
Other nutrients believed to be negatively impacted by statins, Houston says, include carnitine, omega-3s, vitamin E, selenium, creatine and vitamin D. He says that all statin takers should have blood micronutrient tests performed to determine if they have any nutritional deficiencies, and then supplement with the appropriate nutrients. Through discussion with a doctor, reducing the dose of a statin, moving to doses every other day or twice per week, or switching to a water-soluble statin may all help with side effects, he says.
Other problems may arise from the inhibition of cholesterol itself, as well as other natural compounds that we cannot supplement for. It is thought, Houston says, that reducing LDL cholesterol below a certain level in the blood can interfere with downstream processes involving sex hormones, cortisol, aldosterone, DHEA and vitamin D. “Cholesterol is not our enemy. Cholesterol is perhaps one of our most important biochemicals,” Graveline explains, adding, “Cholesterol is vital for proper function of our brain memory centers. Without sufficient cholesterol, memory synapses cannot be laid down.”
Side effects involving emotion and behavior may result from statin-induced dolichol deficiency. “Dolichols are inevitably inhibited with statin use, leading to deficient glycoprotein synthesis. Our neurohormones are derived from this huge glycoprotein class of biochemicals,” Graveline says. Dolichol is critical for not just neurohormone production, but also for cell communication and identification and DNA error correction. It is not available in supplement form. WF
This heart health series is sponsored by
References
1. P. Wehrwein, “Statin use is up, cholesterol levels are down: Are Americans’ hearts benefiting?” http://www.health.harvard.edu/blog/statin-use-is-up-cholesterol-levels-are-down-are-americans-hearts-benefiting-201104151518, accessed July 2, 2012.
2. C.D. Furberg, “Natural Statins and Stroke Risk.” Circulation 99(2), 185–188 (1999).
3. M. Yokoyama, et al., “Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis,” Lancet. 369(9567), 1090-8 (2007).
4. “Triglycerides and How to Lower Them,” WebMD, http://www.webmd.com/cholesterol-management/triglycerides-lowering-triglyceride-levels?page=2, accessed July 2, 2012.
5. B.A. Golomb, “Statin Adverse Effects: Implications for the Elderly,” Geriatric Times, http://www.cmellc.com/geriatrictimes/g040618.html, accessed July 2, 2012.
6. G. Caso, et al., “Effect of coenzyme q10 on myopathic symptoms in patients treated with statins,” Am J Cardiol. 99(10), 1409-12 (2007).
7. J.D. Colbert, J.A. Stone, “Statin Use and the Risk of Incident Diabetes Mellitus: A Review of the Literature,” Can J Cardiol. Epub ahead of print June 4, 2012 (doi:10.1016/j.cjca.2012.03.021).











