Joint pain and swelling is no fun, and unfortunately these issues are way too common. According to the Centers for Disease Control and Prevention, about 52.5 million U.S. adults were diagnosed with arthritis, gout, lupus or fibromyalgia, all of which could reduce joint comfort and mobility (1).
Supplements won’t cure, treat or prevent these issues, but they sure can help keep healthy joints moving comfortably.
Is “Inflammation” A Dirty Word?
Think twice before you discuss “anti-inflammatory” joint supplements with shoppers. That’s the advice from several experts interviewed for this piece.
Let’s back up a moment here. In 2013, the U.S. Food and Drug Administration (FDA) seemed to put companies marketing supplements as anti-inflammatory in the hot seat, with at least 10 warning letters going out (2). Even statements like “supports healthy inflammation response” were problematic.
Some might disagree with FDA’s viewpoint. Cheryl Myers, chief of education and scientific affairs at EuroPharma, Inc., Green Bay, WI (makers of the Terry Naturally brand of products), says many industry experts believe “a strong argument can be made for inflammation as a natural process,” though “FDA has clearly indicated they now consider inflammation to be a disease claim in most cases—even if the claim refers to a ‘healthy inflammation response’ and does not mention a specific disease condition. This should be a reminder that the landscape of acceptable structure/function claims is still evolving.”
Still, FDA calls the shots for what industry can and cannot say about supplements, and compliance is important. Myers believes industry trade groups like the Natural Products Association and the Council for Responsible Nutrition have done “an excellent job of monitoring FDA’s current thinking and disseminating this information to their members and readers.” She suggests retailers join these industry groups to keep abreast of FDA’s current thinking.
So, what can you say to shoppers about inflammation?
Well, for starters, advise shoppers to discuss with their doctors any condition in which chronic inflammation may be involved. But you can say that it is well known that a healthy immune system uses inflammation as a normal way to deal with threats.
Herb Joiner-Bey, N.D., medical science consultant for Barlean’s Organic Oils, Ferndale, WA, says inflammation can occur when tissue is damaged. “To heal, tissue needs to transition through a temporary inflammatory phase that lays the foundation for tissue repair, which is completed during the maturation phase,” he explains.
What happens next? “When the crisis passes, anti-inflammatory mechanisms take over and return the body to its normal condition (homeostasis),” explains Nena Dockery, technical services manager at Stratum Nutrition, St. Charles, MO. She adds that some supplements help maintain this healthy, balanced state or support comfort following exercise.
Michael Mooney, director of research and education at SuperNutrition, Oakland, CA, agrees that “balance” is a good way to explain how supplements can help in the joint health category. “While inflammation sounds like a scary word, it basically means oxidation. So while we cannot talk about ‘inflammation’ in any manner that even hints at treating a disease, we can say that antioxidants work in the body to help keep the inflammatory–anti-inflammatory balance that is required for overall good health,” he states.
“Balance” is also important for understanding inflammation in general. We need it for repair, just not for a  long-term fix, which puts our bodies out of whack. Chronic inflammation is considered a disease state; think conditions like arthritis or Crohn’s disease. “Although not a disease in and of itself, an increasing body of research is showing that when [chronic inflammation] exists in dangerous levels, there is also likelihood of simultaneous disease state,” states Annie Eng, CEO of HP Ingredients, Bradenton, FL. Therefore, she recommends retailers not discuss supplements as “anti-inflammatory” with shoppers.
long-term fix, which puts our bodies out of whack. Chronic inflammation is considered a disease state; think conditions like arthritis or Crohn’s disease. “Although not a disease in and of itself, an increasing body of research is showing that when [chronic inflammation] exists in dangerous levels, there is also likelihood of simultaneous disease state,” states Annie Eng, CEO of HP Ingredients, Bradenton, FL. Therefore, she recommends retailers not discuss supplements as “anti-inflammatory” with shoppers.
Instead, Joiner-Bey says retailers can “offer ideas about ways to support the body’s ability to maintain optimal structure and function of affected tissues. They can say truthfully that the body can utilize constituents of natural products to improve structure and function under challenging conditions through natural biological means.”
Michael Olinde, president of Avie Nutraceuticals, Baton Rouge, LA, agrees. He says that if acute inflammation is happening, it means that the body is beginning the healing process of injured tissue. “While the latter is of no major consequence, the former is likely why the FDA is concerned,” Olinde believes.
Another pitfall to avoid is any discussion about managing disease symptoms. Last month, the WholeFoods Retailer of the Year, Debra’s Natural Gourmet, described how shoppers often come in looking for a second opinion after a doctor’s visit, or a supplement to manage a condition with which they were diagnosed.
“This is where it can be more risky for the retailer to provide helpful guidance without inadvertently making a claim. However, a well-trained retailer can be of great assistance in these cases,” Dockery believes.
Retailers can explain that supplements don’t cure, treat or prevent diseases. But, they can point out specific ingredients with supporting research for joint care, Dockery advises. “Knowledge of ingredients that are supported not only by clinical studies, but also mode of action studies that highlight immunomodulation of the inflammatory process can also be helpful,” she states. “The retailer can explain these benefits to the customer without claiming a treatment of the disease condition.”
 David Foreman, R.Ph., The Herbal Pharmacist, agrees that if retailers discuss any symptoms or risk factors that could be related to a disease state, they should be mentioned generically and not directly about the condition. “Speak generically about the role of inflammation and explain that any word ending in ‘–itis’ means that part of the body is experiencing some sort of inflammation,” Foreman states.
David Foreman, R.Ph., The Herbal Pharmacist, agrees that if retailers discuss any symptoms or risk factors that could be related to a disease state, they should be mentioned generically and not directly about the condition. “Speak generically about the role of inflammation and explain that any word ending in ‘–itis’ means that part of the body is experiencing some sort of inflammation,” Foreman states.
Retailers can also ask manufacturers if their products have any allowable structure/function claims. For instance, Steve Holtby, president and CEO of Soft Gel Technologies, Inc., Los Angeles, CA, says, “A structure/function claim relating to ‘the temporary relief of minor pain’ may be allowable for hops extract: ‘FDA agrees that some minor pain relief claims may be appropriate structure/function claims for dietary supplements. A claim that a product is intended to treat minor pain, without reference to any other conditions, symptoms or parts of the body that would imply disease treatment or prevention, would be an appropriate structure/function claim, because minor pain, by itself, can be caused by a variety of conditions, not all of them disease-related’ [65 Fed. Reg. 1000, 1030, Jan. 6, 2000].”
Another strategy is to talk about diet. “Our industry should do a better job helping our customers know there are foods that actually cause inflammation, so consuming plenty of anti-inflammatory foods is an important first step,” believes Lou Paradise, president and chief of research at Topical BioMedics, Inc., Rhinebeck, NY. He says these include vegetables, fruits, whole grains and fish rich in omega-3 fatty acids, as well as nuts and legumes. He also suggests stores offer a modified grocery list and recipes to emphasize these foods.
Conversely, Paradise says retailers can point out that processed foods with white sugar, artificial sweeteners and hydrogenated fats are linked to inflammation.
“Reassure customers that they did not get these issues overnight and as much as making changes can be a challenge, most people see noticeable results that lead to a more vibrant, healthier, active lifestyle in a short period of time. That is a motivating reward!” says Paradise.
The Cellular Connection
So, how does inflammation work? The basic components of an inflammatory response are: vasodilation for increase blood flow into the capillaries, leakier capillaries (which causes swelling) and white blood cells, which rush to the scene of tissue damage. Such cells include monocytes (which become macrophages), lymphocytes (like B cells, T cells and NK cells), short-lived neutrophils, dendritic cells and more. When these white blood cells stick around too long, chronic inflammation can include “fluid buildup, heat and redness, joint pain, stiffness and loss of joint function,” states Holtby.
Tumor necrosis factor-alpha (TNF-alpha) and cyclooxygenase-2 (COX-2) are two of many proteins that play roles in activating immune cells and inflammation. For this reason, companies interested in tackling the roots of joint pain have focused on these compounds. This includes drug companies.
 “Today, the study of inflammation has gone from the tissue levels deeper into the nuclear level. Cell-signaling molecules have been identified which stimulate the genes that induce the expression of the COX enzyme which in turn induce inflammation,” states Shaheen Majeed, marketing director at Sabinsa Corp., East Windsor, NJ.
“Today, the study of inflammation has gone from the tissue levels deeper into the nuclear level. Cell-signaling molecules have been identified which stimulate the genes that induce the expression of the COX enzyme which in turn induce inflammation,” states Shaheen Majeed, marketing director at Sabinsa Corp., East Windsor, NJ.
Some of the most common ways to treat joint pain is with non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen or naproxen and corticosteroids. While it isn’t a retailer’s job to tell shoppers which medications they should and shouldn’t take, it is worth knowing that NSAIDs have been linked to numerous side effects. In fact, in July, FDA moved to strengthen some warnings on NSAIDs. Prescription NSAID labels must now tell shoppers that the drugs increase the risk of stroke and heart attacks, even as early as the first weeks of use. The risk grows at higher doses, according to FDA’s research.
States Holtby, “Unfortunately, NSAIDs aren’t selective; they inhibit both COX-1 and COX-2 enzymes with varying intensity.” This is a problem because while blocking COX-2 may reduce pain, inhibiting COX-1 is rarely a good thing. This enzyme’s job is to protect the gastrointestinal (GI) tract lining. According to Holtby, “As a result, GI-related adverse events are common, resulting in an estimated 103,000 hospitalizations and 16,500 deaths per year in the U.S.”
While drug companies started marketing selective COX-2 inhibitors, which would block COX-2 enzymes but not COX-1, their side effects were worse. As a result, drugs like Vioxx were pulled from the market for their links to heart attack and stroke. Says Holtby, “The problem was that they were too selective. By completely shutting down COX-2, these drugs are theorized to suppress production of the blood-clotting hormone prostacyclin and other cardio-protective enzymes, thus increasing cardiovascular events.”
Now while herbs are not drugs, and cannot treat inflammation, there has been some compelling research suggesting that they affect COX-2 and COX-1, but in ways that don’t harm the body.
For instance, one patented hops extract (Perluxan from Soft Gel Technologies) is said to offer benefits to those looking for joint comfort, without the side effects commonly associated with prescription anti-inflammatory products. States Holtby, “The subject of multiple in vitro, ex vivo and in vivo human clinical trials (3), Perluxan moderately inhibits COX-2 and mildly inhibits COX-1, and is well-tolerated and does not cause GI distress.”
In one human trial, researchers found that Perluxan provided relief in subjects with occasional knee discomfort, increasing knee function and better quality of life (4).
Other herbs may also affect enzymes in a way that supports healthy joint tissues. “Take Pycnogenol for instance,” says Carolina Burki-Sozzi, director of product development at Horphag Research, Geneva, Switzerland (worldwide exclusive supplier of Pycnogenol). “Years of research has found that those who supplement daily with the super antioxidant generate less matrix metalloproteinase (MMP) enzymes, which are responsible for degenerating cartilage collagen in osteoarthritis,” she  explains.
explains.
Dockery explains that MMP enzymes are responsible for normal functions as they break down certain proteins in support of healthy tissue remodeling. “However, they are also involved in disease processes,” Dockery states. “For example, MMP-3 degrades several types of collagen, including collagen type II, as well as other substances within the joint and surrounding connective tissue integral to healthy cartilage structure.”
That’s not the only way Pycnogenol supports healthy joints. According to Burki-Sozzi, the herb stimulates the production of hyaluronic acid and collagen, which are key for healthy joints. In addition, she states, “Pycnogenol consumption was found to naturally decrease the expression of 5-LOX and COX-2 in humans further contributing to decrease the inflammation and providing a significant contribution for lowering joint pain.”
In one clinical trial with 156 osteoarthritis patients, three months of supplementing with Pycnogenol slashed pain scores and patients’ use of NSAIDs by 58%. Mobility also increased (5).
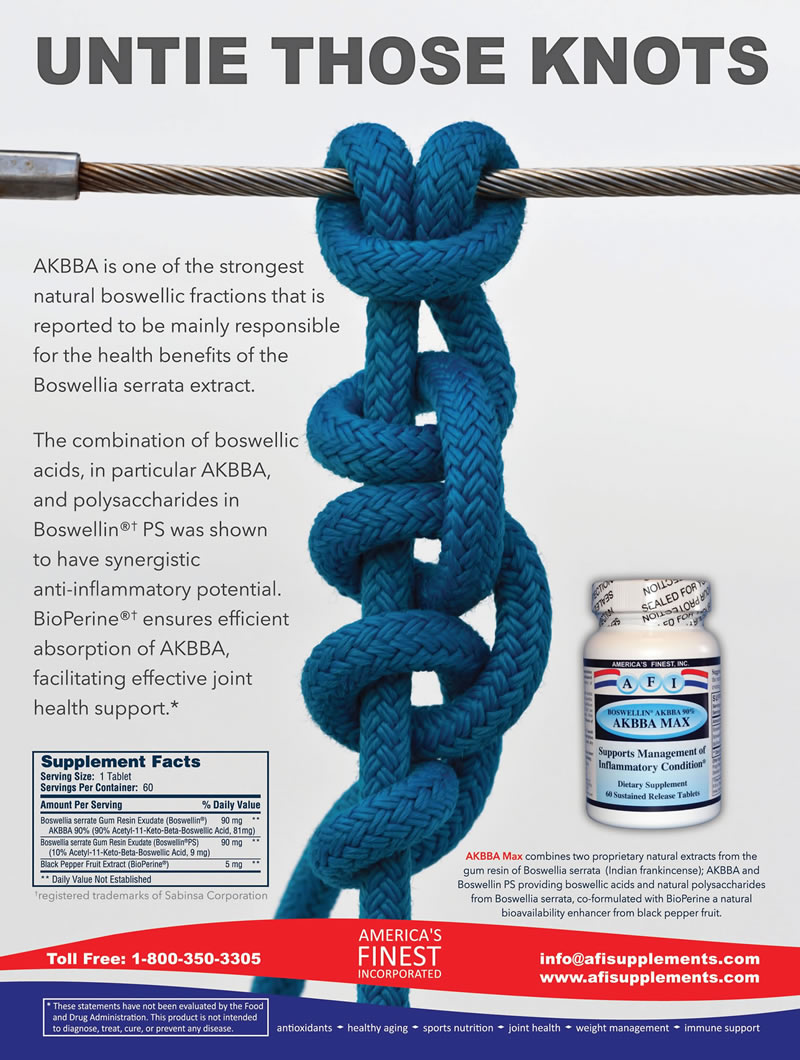
Boswellia serrata is another ingredient with ties to inflammatory enzymes. Aparna Kalidindi, Pharm.D., BCPS, technical sales and marketing manager at Natreon, Inc., New Brunswick, NJ, explains the link: “It inhibits inflammatory factors and the COX enzyme pathway; thus, leading to a reduction in inflammatory prostaglandins. It also acts as an analgesic and may improve circulation to damaged joints and inflamed tissue.”
A branded form from her company (Natreon’s AyuFlex) was found in studies to decrease WOMAC and VAS scores for pain and knee swelling significantly in moderately osteoarthritic subjects. “It also increases pain threshold force and pain tolerance force in healthy volunteers. In addition to joint health benefits, AyuFlex is a super antioxidant with ORACFN value of 36,000 µmoles TE/g.”
Another branded form (5-Loxin from PLT Health Solutions) has had a positive effect on markers of inflammation (like TNFa, CRP and IL-6), and is said to inhibit MMP-3 enzymes. In one study, this ingredient and another boswellia extract both improved knee pain and function in a group of 57 patients (6).
Astaxanthin may also inhibit some pro-inflammatory compounds. According to Janice Brown, technical sales support at AstaReal USA, Burlington, NJ, her company’s branded form (AstaReal) has research backing suggesting it supports a healthy inflammatory response.
“AstaReal was issued a patent for astaxanthin as method of inhibiting the expression of inflammatory  cytokines and chemokines, the very protein biomarkers that signal the onset of the inflammatory cascade,” says Brown. “Astaxanthin was shown in other studies to alleviate muscle and joint soreness and promote faster recovery from exercise-induced muscular fatigue.”
cytokines and chemokines, the very protein biomarkers that signal the onset of the inflammatory cascade,” says Brown. “Astaxanthin was shown in other studies to alleviate muscle and joint soreness and promote faster recovery from exercise-induced muscular fatigue.”
Another branded extract, this time of Andrographis paniculata (ParActin), is said to support healthy joint function and muscle health. In one study, 60 rheumatoid arthritis patients took 100 mg of ParActin or a placebo three times a day for 14 weeks; everyone was given methotrexate as a standard treatment and prednisone was allowed (7). According to Eng, ParActin reduced the number of swollen joints, total grade of swollen joint and tender joints; pain and the intensity of rigidity also were reduced.
Individuals also had lower levels of c-reactive protein from above normal (over 3% at pre-treatment) to a normal level of 0.5%. “ParActin also help to normalize rheumatoid factor, creatine kinase, hemoglobin, immunoglobin IgA and IgM,” states Eng. “The reduction in IgA and IgM is beneficial as there is positive correlation between the grade of cartilage damage.”
The herbs mentioned here just scratch the surface of the hundreds of botanicals that have been researched to support joint comfort. According to Holtby, “Scientists discovered many herbs that can safely, powerfully, and naturally inhibit the COX-2 enzyme. Those herbs include green tea, ginger, turmeric, holy basil, chamomile, Chinese goldthread, barberry, Baikal skullcap, Hu zhang (Japanese knotweed), rosemary, hops, feverfew and oregano.”
While not an herb, eggshell membrane supports healthy joint structure though its content of collagen (several types), glycosaminoglycans (GAGs) such as hyaluronic acid and chondroitin sulfate, as well as glucosamine, beneficial proteins and peptides. In addition, Dockery notes that two in vitro and one animal study suggest the branded NEM (natural eggshell membrane) reduces the pro-inflammatory agents cytokines. Cytokines (like interleukin) help regulate how the immune system responds to inflammation and infection.
In one lab study on NEM, human cells were exposed to a substance known to cause a simple T-cell  immune response and another substance that elicits a more complex immune response. Both involve the release of pro-inflammatory cytokines (8). According to Dockery, “The results revealed that NEM could indeed modulate the immune response by decreasing levels of the pro-inflammatory cytokines. The digestive process did not interfere in NEM’s activity; and even enhanced the inhibiting effects on levels of the pro-inflammatory cytokine, TNF-a in the more complex immune response.”
immune response and another substance that elicits a more complex immune response. Both involve the release of pro-inflammatory cytokines (8). According to Dockery, “The results revealed that NEM could indeed modulate the immune response by decreasing levels of the pro-inflammatory cytokines. The digestive process did not interfere in NEM’s activity; and even enhanced the inhibiting effects on levels of the pro-inflammatory cytokine, TNF-a in the more complex immune response.”
A separate animal study bolstered these results, showing that NEM provides “in vivo support for the reduction of multiple circulating pro-inflammatory cytokines, particularly IL-1b and TNF-a following oral supplementation with NEM in both healthy rats and inflammatory-challenged rats (9). Dosing in the animal study supported the human equivalent dosing of 500 mg/day.”
Problem Solved: Curcumin Absorption
A big player in the joint health category is curcumin, which also may affect proinflammatory agents in the body. According to Majeed, “Curcuminoids from rhizomes of Curcuma longa are an inhibitor of NF- kB, the master regulator of inflammation.”
He calls NF-kB—or Nuclear Factor-Kappa B—the “master switch” for adjusting inflammation, which underscores why inhibiting it may play a role in joint comfort.
But, there has been some criticism that this nutrient is difficult for the body to absorb. “As of October 2014, more than 5,000 scientific studies have focused on curcumin. Its primary biological effects relate to its action as a broad-spectrum antioxidant and profound anti-inflammatory agent,” states Michael T.  Murray, N.D., director of product science and innovation at Natural Factors Nutritional Products, Inc., Monroe, WA. “However, its use in clinical trials has been limited due to poor oral absorption in humans.”
Murray, N.D., director of product science and innovation at Natural Factors Nutritional Products, Inc., Monroe, WA. “However, its use in clinical trials has been limited due to poor oral absorption in humans.”
Majeed says using biotransformed curcumin is one way companies are dealing with this problem. He explains that once curcumin reaches the gastrointestinal tract, it undergoes microbial transformation and forms various metabolites.
In a study from PNAS, the microbial metabolism of curcumin has a two-step reduction, with curcumin converted NADPH-dependently into dihydrocurcumin, and then, tetrahydrocurcumin (THC), tetrahydrodemethoxycurcumin (THDMC) and tetrahydrobisdemethoxycurcumin (THBDMC) (10). The actions of other enzymes in the body form metabolites such as hexahydrocurcumin, octahydrocurcumin, curcumin glucuronides, curcumin sulphates and ferulic acid (11–13).
Majeed says his company offers a curcumin extract with at least 95% tetrahydrocurcuminoids (C3 Reduct) for enhanced bioavailability. The company also combines curcumin (Curcumin C3 Complex) and a Piper nigrum extract (BioPerine). He states, “BioPerine has been clinically studied for increasing the bioavailability of several nutrients including curcuminoids.”
Mooney says his firm uses the latter option—95% curcuminoids with black pepper extract (as BioPerine)—in a combination product with glucosamine and MSM for its performance and cost effectiveness. “Our main considerations were cost versus benefit and getting the most effectiveness in the least amount of tablet space,” he explains, adding that the curcumin ingredient “has been shown to safely improve blood levels and extend the absorption and bioavailablity of curcumin tremendously.”
These aren’t the only ways companies are innovating with curcumin. According to Myers, “There are several ways to boost curcumin absorption, but this is a topic of real contention. Researchers can’t agree on what to test to determine absorption, or which laboratory methods to use.”
She adds that some companies use “synthetic, unhealthy solvents” to boost absorption, but she questions the safety of this technique. She also says some curcumin products incorporate several curcuminoids, while others do not.
|
Select Joint Comfort Products Anderson Global Group: Provinal. AstaReal, Inc.: AstaREAL natural astaxanthin, available in 10% oil, 2% powder, 1.5% water soluble liquid, and 2–6-mg finished softgels. Retail line includes Astavita Sport, Astavita Smooth, Astavita Astaxanthin + BCAA and more. Avie Nutraceuticals: Joint Balance. Barlean’s Organic Oils: Barlean’s Omega Swirl Fish Oil, Barlean’s Omega Swirl Flaxseed Oil and Barlean’s Joint Remedy. EuroPharma, Inc.: CuraMed (capsules, softgels and effervescent tablets), Cherry Fruit, Tart Cherry, Healthy Knees & Joints and more. Horphag Research: Worldwide exclusive supplier of Pycnogenol. HP Ingredients: ParActin. Natreon Inc.: AyuFlex. Natural Factors Nutritional Products, Inc.: CurcuminRich Theracurmin, CurcuminRich Double Strength Theracurmin, RxOmega-3, Pycnogenol Pine Bark, CherryRich Super Strength and BlueRich Blueberry. Neptune Technologies and Bioressources Inc.: NKO softgels (500 and 1,000 mg); NKO FLEX. OptiPure: IncaCartilago. P.L.T. Health Solutions: 5-Loxin. Proprietary Nutritionals Inc.: Celadrin, Vege-Celadrin. Sabinsa Corp.: Boswellin, Curcumin C3 Complex, Ginger Extract. Soft Gel Technologies, Inc.: Perluxan, Injuv (HA complex) with Glucosamine, several potencies of Vitamin D in soft gelatin capsules, EZ Mega 3 softgels, Cod Liver Oil, CoQ10 (including CoQsol, CoQsol-CF and CoQH-CF). Stratum Nutrition: NEM (Natural Eggshell Membrane). SuperNutrition: SuperNutrition Glucosamine and MSM. Topical Biomedics: Topricin Original, Topricin Foot Therapy, and Topricin for Children. |
“Since all curcumin is not created equal, this is an area where it pays to do your homework,” says Myers.
Her favorite is a branded form (BCM-95 Curcumin, from Dolcas Biotech, in CuraMed) that has much clinical backing (24 published trials) and offers enhanced curcumin absorption. “The patented method to improve absorption and efficacy is by impregnating the curcumin flakes with turmeric essential oil,” she explains. “This leads to significantly better absorption, but the healthy compounds in turmeric essential oil, most notably the turmerones, boosts curcumin’s activity systemically for more profound benefits. CuraMed contains curcumin that contains turmeric essential oil and turmerones in a patented formulation.”
In the case of Avie Nutraceuticals, another technique is to reduce curcumin’s particle size with an ultramicronization process.
Olinde says when curcumin products do not dissolve easily, the curcumin is less likely to be well absorbed. An ultramicronized formula, he believes, solves this problem. “This technologically advanced process (which is new) renders curcumin in its natural form to dissolve in water, therefore allowing quick absorption,” he states. “Our researchers have revealed that our ultramicronized curcumin is 352 times greater in antioxidant activity than comparisons; has more than 1,400 times greater free radical scavenging properties, and has 126 times greater inhibition of cyclooxygenase-2 (COX-2).”
Murray also believes that reducing curcumin’s particle size is the way to go, and his favorite form for increasing levels of curcumin in the blood is Theracurmin (from Theravalues, Tokyo, Japan). “Theracurmin is a powdered colloidal mixture produced by reducing the particle size of curcumin by over 100 times and emulsifying it within a natural vegetable gum to improve solubility and absorption,” he explains.
Not only does this technique improve absorption, but it also “stays in the blood far longer than any other commercial form of curcumin,” he feels.
In 2014, researchers from Kyoto Medical Center gave 50 patients with osteoarthritis of the knee the branded curcumin (180 mg/day) or a placebo for eight weeks. At the end of the study, knee pain VAS scores were significantly lower in the curcumin group; these patients were also able to lower their dependence on NSAIDs more than the placebo group (14).
Omegas for Joints
With all this talk about inflammation, one would be remiss not to bring omegas into the discussion.
Dockery reminds us that key to the discussion are omega-6 fatty acids, which produce pro-inflammatory arachidonic acid, and omega-3s like EPA and DHA, which have had anti-inflammatory effects in studies. She says that studies in those with arthritis suggest that omega-3s work by decreasing the levels of pro-inflammatory cytokines and matrix metalloproteinases. “Unfortunately, the ratio of omega-6 fatty acids to omega-3 fatty acids in the Western diet is disproportionately composed of omega-6 fatty acids, potentially contributing to an increase in diseases linked to chronic inflammation,” Dockery states.
Michael De Cicco, M.Sc., product technical support specialist at Neptune Technologies and Bioressources Inc., Laval, Canada, agrees, stating, “The human body should have an optimal ratio of 1:1 omega-6 to omega-3, if not lower, in order to beneficially reduce inflammation and thus improve joint comfort…A high omega-6 to omega-3 ratio tends to promote inflammatory pathogenesis such as rheumatoid arthritis and osteoarthritis.”
Joiner-Bey explains that omega-3s produce compounds called resolvins and protectins, which help to  decrease inflammation and protect the joints. “These hormones that control and shut down inflammation naturally cannot be manufactured by cells in the absence of the omega-3 EPA, as in fish oil, or its precursor ALA, as in flax oil,” he explains. To this, Foreman adds another mechanism of action: it inhibits COX.
decrease inflammation and protect the joints. “These hormones that control and shut down inflammation naturally cannot be manufactured by cells in the absence of the omega-3 EPA, as in fish oil, or its precursor ALA, as in flax oil,” he explains. To this, Foreman adds another mechanism of action: it inhibits COX.
These actions combine to help keep the body’s inflammation response in healthy balance for optimal joint comfort, among other things. “Several studies have been published reviewing the effectiveness of omega-3 fatty acids in combating inflammatory conditions, such as arthritis,” Kalidindi states. “In one study, researchers found that 300 mg of krill oil supplementation daily significantly reduced inflammation, pain, stiffness, and function impairment after just seven days.”
The study she describes involved 90 people who were diagnosed with cardiovascular disease, rheumatoid arthritis or osteoarthritis. Individuals took 300 mg of krill oil (as NKO from Neptune) or a placebo for a month. After a week, the krill oil reduced C-reactive protein levels by 19%; those taking the placebo saw a 16% increase. By the study’s end, C-reactive protein was reduced 31% in those taking krill oil. Moreover, after a week of taking krill oil, individuals had reduced pain scores (by 29%), reduced stiffness (by 20%) and functional impairment (by 23%) (15).
In addition to omega-3s, Joiner-Bey believes palmitoleic acid supports a balanced inflammation response. “The monounsaturated omega-7 palmitoleic acid has always been a constituent of fish oil,” he states. “Although it is not considered to be an EFA, this omega-7 has been recently concentrated from fish oil to produce a supplement that is extremely effective in reducing a biomarker for inflammation (c-reactive protein or CRP). In fact, palmitoleic acid reduces CRP better that any other tested nutrient.”
In one study, a branded form of omega-7 (220.5 mg as Provinal, distributed by Anderson Global Group, Irvine, CA) or a placebo was given to adults with high cholesterol and evidence of systemic inflammation. After 30 days, the omega-7 group experienced reductions in c-reactive protein (by 44%), triglyceride (15%) and LDL (8%) levels (16).
A last ingredient (Celadrin from Proprietary Nutritionals Inc.) to consider in this category is a unique fatty acid that “works much like essential fatty acids EPA and DHA from omega-3 fish oils, but with a much more dramatic result because it causes change at the body’s cellular level,” states Dean Mosca, president of Proprietary Nutritionals Inc., Kearny, NJ.
This ingredient, he explains, is made through a proprietary process of esterifying fatty acids. This technique is said to ensure stability and prevent oxidative reactions. For joint health, Mosca says the  ingredient has been found in human studies to lessen pain and swelling and increase range of motion. “It works by decreasing inflammation and lubricating cell membranes throughout the body, restoring fluids that cushion bones and joints to promote flexibility and mobility,” Mosca states.
ingredient has been found in human studies to lessen pain and swelling and increase range of motion. “It works by decreasing inflammation and lubricating cell membranes throughout the body, restoring fluids that cushion bones and joints to promote flexibility and mobility,” Mosca states.
At the cellular level, this branded ingredient has been found to lessen the effects of pro-inflammatory effects of arachidonic and other fatty acids by reducing the production of IL-6.
Anthocyanins for Joint Support
Some of the most impressive antioxidants for joint support come by way of anthocyanidins sourced from fruits. Says Murray, “Cherries, blueberries and other dark red and blue berries are rich sources of anthocyanidins and proanthocyanidins. These compounds are flavonoid molecules, which give these fruits their deep red-blue color, and are remarkable in their ability to prevent collagen destruction.”
Anthocyanidins and proanthocyanidins, says Dockery, have both anti-inflammatory and potent antioxidant characteristics and benefit healthy cartilage. “In osteoarthritis, there is often an enhanced expression of the pro-inflammatory cytokine, interleukin-1b (IL-1b). Anthocyanins have been shown in some studies to inhibit IL-1b production of certain cartilage-degrading molecules,” she explains.
In addition to inhibiting collagen-destroying enzymes, Murray explains that they can cross-link collagen fibers, “resulting in reinforcement of the natural cross-linking of collagen that forms the collagen matrix of connective tissue (e.g., ground substance, cartilage, tendon).” He adds that in addition to preventing the release of IL-1b, they also inhibit histamine, serine proteases, prostaglandins and leukotrienes.
Myers says a recent analysis of data from the Framingham Heart Study Offspring cohort suggests anthocyanins affect 12 inflammatory biomarkers (17). “Results showed that higher anthocyanin intake (from foods, in this case) accounted for a 73% lower overall inflammation score between the highest and lowest quintile categories,” she states, noting that lifestyle choices also play a major role in one’s inflammation levels.
Kalidindi says tart cherries “may be the best source.”
According to Myers, cherries and cherry juice have been a traditional remedy for gout, a disease that causes joint pain due to uric acid crystals accumulation. “Cherries have been shown in clinical studies to  reduce excessive uric acid levels,” she explains.
reduce excessive uric acid levels,” she explains.
Additionally, bioflavonoids that support balanced inflammation include quercetin, resveratrol and polyphenols according to Holtby.
To this list, Murray adds Pycnogenol and grape seed extracts, which contain flavonoids called procyanidolic oligomers (PCOs) or oligomeric proanthocyanidins (OPCs).
Myers calls OPCs “crucial for optimal joint function,” particularly formulations developed for optimal absorption.
According to Murray, taking 100–300 mg/day of PCOs for six weeks was found in studies to considerably improve the serum total antioxidant capacity and oxygen radical absorbance capacity score (ORAC). “Grape seed and/or pine bark extract have also shown significant benefits in clinical studies including several health conditions associated with inflammation including osteoarthritis,” he states.
On the Surface
Shoppers may be interested to know whether topical formulas may work well for joint support. But, several experts say that creams may not be the best format for inflammation support. According to Joiner-Bey, inflammation happens at the cellular/tissue level. “Therefore, the most effective interventions must be directed from the inside out, not the outside in. Topical preparations may provide a little relief at best, but they can never resolve the underlying cause,” he states.
Paradise agrees, noting, “The molecular structure of most nutrients is too large to be effectively absorbed through the skin, or get enough absorption to have any effect. It is tough enough to get good absorption through the gut, because of bioavailability challenges that starts with the digestive health of the person needing to supplement.”
But that doesn’t mean you should disband your topical support section. Far from it, actually. Certain compounds may be appropriate for some nutrients. According to Majeed, “Ingredients such as boswellic acids from Boswellia serrata gum have been evaluated and found to offer relief through its anti-inflammatory activity through both topical as well oral routes.”
He says this may also be the case with ginger extract and curcuminoids. “The understanding of the specific molecular targets and mechanisms of actions of these phytonutrients in offering joint support may be attributed to their application through diverse dosage forms,” Majeed states.
Topical formulas also have another valuable role to play: support for soreness after exercise. Next month, we round out our Bone and Joint series with coverage of joint support for athletes, which will include a discussion of the role of topical products. WF
References
1. Centers for Disease Control and Prevention, “Arthritis-Related Statistics,” www.cdc.gov/arthritis/data_statistics/arthritis_related_stats.htm, accessed Aug. 3, 3015.
2. Alliance for Natural Health, “The FDA Calls One of the Body’s Basic Healing Functions a ‘Disease,’” www.anh-usa.org/inflammation-disease, accessed Aug. 3, 3015.
3. M. Lemay et al., “A Dietary Supplement Is a Selective COX-2 Inhibitor Both In Vitro and Ex Vivo In Healthy Human Volunteers,” Nutrilite Health Institute, Access Business Group LLC, Buena Park CA.
4. R. Jager and M. Purpura, “Efficacy of Oral Perluxan Intake: A Randomized, Double-Blind Study,” Pharmachem Laboratories, Kearny, NJ.
5. G. Belcaro, et al., “Treatment of Osteoarthritis with Pycnogenol. The SVOS (San Valentino Osteo-Arthrosis Study). Evaluation Of Signs, Symptoms, Physical Performance And Vascular Aspects,” Phytother. Res. 22: 518–523 (2008).
6. K. Sengupta et al., “Comparative Efficacy And Tolerability Of 5-Loxin And Aflapinagainst Osteoarthritis Of The Knee: A Double Blind, Randomized, Placebo Controlled Clinical Study,” Int. J. Med. Sci. 7 (6), 366–377 (2010).
7. R.A. Burgos, et al., “Efficacy of an Andrographis Paniculata Composition for the Relief Of Rheumatoid Arthritis Symptoms: A Prospective Randomized Placebo-Controlled Trial,” Clin. Rheumatol. 28 (8), 931-946 (2009).
8. K.F. Benson, K.J. Ruff and G.S. Jensen, “Effects of Natural Eggshell Membrane (NEM) on Cytokine Production in Cultures of Peripheral Blood Mononuclear Cells: Increased Suppression of Tumor Necrosis Factor-a Levels After In Vitro Digestion,” J. Medic. Food, 15 (4), 360–368 (2012).
9. K.J. Ruff and D.P. DeVore, “Reduction of Pro-Inflammatory Cytokines In Rats Following 7-Day Oral Supplementation With A Proprietary Eggshell Membrane-Derived Product,” Mod. Res. Inflamm. 3 (1), 19–25 (2014).
10. A. Hassaninasab, et al., “Discovery of the Curcumin Metabolic Pathway Involving A Unique Enzyme In An Intestinal Microorganism,” PNAS 108 (16), 6615-6620 (2011).
11. P. Anand, et al., “Biological Activities of Curcumin and its Analogues (Congeners) Made By Man and Mother Nature,” Biochemical Pharmacology. 76, 1590–1611 (2008).
12. J.K. Lin, et al., “Recent Studies on the Biofunctions and Biotransformations of Curcumin,” Biofactors. 13, (1–4) 153–158 (2000).
13. C.R. Ireson, et al., “Metabolism of the Cancer Chemopreventive Agent Curcumin in Human and Rat Intestine,” Cancer Epidemiol. Biomarkers Prev. 11 (1), 105–111 (2002).
14. Y. Nakagawa, et al., “Short-Term Effects Of Highly-Bioavailable Curcumin For Treating Knee Osteoarthritis: A Randomized, Double-Blind, Placebo-Controlled Prospective Study,” J. Orthop. Sci. 19 (6), 933–939 (2014).
15. L. Deutsch, “Evaluation of the Effect of Neptune Krill Oil on Chronic Inflammation and Arthritic Symptoms,” J. Am. Coll. Nutr. 26 (1), 39–48 (2007).
16. A.M. Bernstein, M. Roizen and L. Martinez, “Purified Palmitoleic Acid for the Reduction of High-Sensitivity C-Reactive Protein and Serum Lipids: A Double-Blinded, randomized, Placebo Controlled Study,” J. Clin. Lipidol. 8 (6), 612–617 (2014).
17. A. Cassidy, et al., “Higher Dietary Anthocyanin and Flavonol Intakes Are Associated With Anti-Inflammatory Effects In A Population Of US Adults, Am. J. Clin. Nutr. 102 (1), 172–181 (2015).
Published in WholeFoods Magazine, September 2015