Now that most scientists recognize that cardiovascular heart disease results from inflammation in the arteries (which leads to plaque that can rupture and cause an acute heart attack or stroke), a new test has been developed that strongly depicts an individual’s risk of this disease. As it has turned out, the Omega-3 Index test is an extremely strong and accurate predictor of heart disease risk.
The Omega-3 Index test is a simple blood test that examines the levels of certain fatty acids in red blood cells. The Index reflects the cellular content of the primary omega-3 fatty acids in fish oil. The Omega-3 Index is measuring a factor that both predicts future risk for a disease and can be altered by a lifestyle (diet) change. Making the changes suggested by the Omega-3 Index will change the risk for developing a disease. This month, we talk with Dr. William Harris, Ph.D. about this important test.
Dr. William Harris holds a Ph.D. in nutritional biochemistry from the University of Minnesota and he completed post-doctoral research with Dr. William Connor at the Oregon Health Sciences University. He  was director of the Lipid Research Laboratories at the University of Kansas Medical Center (KUMC) and at the Mid America Heart Institute, both in Kansas City, MO, for 22 years, and was on the faculty at KUMC and at the University of Missouri-Kansas City School of Medicine. Between 2006 and 2011 was the director of the Cardiovascular Health Research Center at Sanford Research/USD (Sioux Falls, SD). Over the last 32 years, Dr. Harris’s research has focused primarily on omega-3 fatty acids and cardiovascular disease. He has been the principal investigator on five omega-3 related NIH grants, and is currently evaluating omega-3 blood tests as a possible new risk factor for cardiovascular disease. In 2004, he and his colleague Clemens von Schacky proposed that the “omega-3 index” be considered as a new cardiovascular risk factor, and in 2009 he founded a company (OmegaQuant, LLC) to offer the test commercially. In 2011, he became director of research and clinical trials at Health Diagnostic Laboratory, Inc. (Richmond, VA). He retains an academic appointment as research professor of medicine at the Sanford School of Medicine, University of South Dakota in Sioux Falls.
was director of the Lipid Research Laboratories at the University of Kansas Medical Center (KUMC) and at the Mid America Heart Institute, both in Kansas City, MO, for 22 years, and was on the faculty at KUMC and at the University of Missouri-Kansas City School of Medicine. Between 2006 and 2011 was the director of the Cardiovascular Health Research Center at Sanford Research/USD (Sioux Falls, SD). Over the last 32 years, Dr. Harris’s research has focused primarily on omega-3 fatty acids and cardiovascular disease. He has been the principal investigator on five omega-3 related NIH grants, and is currently evaluating omega-3 blood tests as a possible new risk factor for cardiovascular disease. In 2004, he and his colleague Clemens von Schacky proposed that the “omega-3 index” be considered as a new cardiovascular risk factor, and in 2009 he founded a company (OmegaQuant, LLC) to offer the test commercially. In 2011, he became director of research and clinical trials at Health Diagnostic Laboratory, Inc. (Richmond, VA). He retains an academic appointment as research professor of medicine at the Sanford School of Medicine, University of South Dakota in Sioux Falls.
Passwater: When did you become interested in omega-3 fatty acids and heart disease?
Harris: In 1979, while I was at the Oregon Health Sciences University, Portland. My postdoc mentor (Professor Bill Connor) assigned me to design and carry out a study in the metabolic ward with healthy volunteers to see how salmon oil would affect cholesterol levels in comparison with animal fats and vegetable oils. We knew hard fats from animals raised cholesterol, liquid oils from plants lowered cholesterol, but what would liquid oils from an animal do to the lipid profile? We were not specifically focusing on EPA and DHA at the time, more the highly polyunsaturated-ness of the oils. We learned about Drs. Jørn Dyerberg and H.O. Bang’s work in Greenland Inuit in the midst of our study and started to think more about the omega-3s in particular, and how they might be unique. This led to studies on platelet function that were carried out in the same volunteers.
Passwater: That’s just about the same time I learned of Dr. Dyerberg’s research. When did you realize that a measurement of omega-3s in the blood could be an indicator of heart disease risk? What was the “eureka” moment?
Harris: The eureka moment took place in November 2002 in the bar at the McCormick Place in Chicago. I was having a drink with a fellow omega-3 researcher from Munich (Dr. Clemens von Schacky), and we were musing about new studies that were showing links between red blood cell (RBC) omega-3 levels and sudden cardiac death. That’s when it occurred to us that we should be viewing the omega-3 levels as risk factors, not just markers of fish intake. We fantasized about creating a new business selling such a test, him in Europe and me in the United States. We’d share methodologies (since the test results are very method specific) and try to have our new risk factor universally accepted. I went on to formalize the laboratory method and to start a business called OmegaMetrix, LLC in the United States, and later, Clemens did the same, founding OmegaMetrix EU. My original company (in Kansas City) ultimately failed for lack of capital (and a myriad of other reasons), whereas his kept going. I restarted the business under the name OmegaQuant, LLC is Sioux Falls, SD in 2009. Dr. von Schacky and I continue to collaborate, and are both helping a company called OmegaQuant Asia get started in Seoul, Korea. By the way, the term “HS-Omega-3 Index” is the proprietary test that we offer, and the “HS” refers to Harris and von Schacky.
Passwater: What does the HS-Omega-3 Index measure?
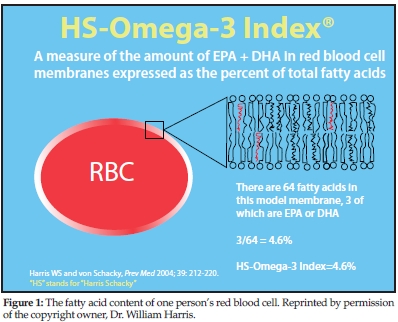
Harris: The fatty acid content of RBC. Figure 1 depicts a RBC with a section of its lipid bilayer expanded to show membrane phospholipids. Each of the 32 phospholipid molecules shown here has two fatty acids (FA); those in red are the long-chain omega-3 FA EPA and/or DHA. With a total of 64 FA, three long-chain omega-3 FA constitute 4.6% of the total FA. Hence, the Omega-3 Index of the patient from whom this cell was taken would be 4.6%.
Passwater: What is the advantage of using RBC for the measurement?
Harris: RBC omega-3 levels are 1) more biologically stable (i.e., they don’t vary hardly at all within each person from week to week), 2) technically easier to analyze than plasma or plasma phospholipids, 3) reflective of long-term omega-3 intake, 4) well-studied and linked with risk for major diseases, 5) well-
correlated with most other metrics of omega-3 status.
Passwater: What studies have you done using the Omega-3 Index and what did you find?
Harris: We found many things. A list of my publications on or referring to the omega-3 index is appended. We found that:
1. the Omega-3 Index was only partly determined by the omega-3 intake and that person to person differences were not even 50% explained by differences in intake;
2. an Omega-3 Index of >8% was associated with a lower risk for acute coronary syndromes (ACS). ACS is an umbrella term used to cover any group of clinical symptoms compatible with acute myocardial ischemia. Acute myocardial ischemia is chest pain due to insufficient blood supply to the heart muscle that results from coronary artery disease (also called coronary heart disease);
3. a suite of 10 RBC fatty acids (including omega-3, omega-6, saturated and trans-fatty acids) could discriminate between ACS patients and controls better than the standard risk factors (age, sex, smoking, cholesterol, HDL, blood pressure and diabetes);
4. a higher Omega-3 Index was associated with slowed “cellular aging” as measured by the five-year rate of telomere shortening;
5. heart patients with below average Omega-3 Index values died at a faster rate than those with above average levels;
6. patients with severe sleep apnea have lower RBC DHA levels than people who have less severe disease;
7. patients admitted to the hospital with an acute MI are less likely to develop ventricular arrhythmias if they have a higher versus a lower Omega-3 Index;
8. inflammatory markers were inversely related to the Omega-3 Index;
9. older people seem to have higher Omega-3 Index values than younger people;
10. a lower Omega-3 Index was associated with depression, both in adolescent patients and in post ACS patients;
11. a slower heart rate was related to a higher Omega-3 Index; and
12. the Omega-3 Index was directly associated with cardiac exercise parameters in patients with stable coronary heart disease (CHD)
With more to come…
Passwater: How does the Index compare to other common risk indicators (specifically blood cholesterol) as an indicator of future heart disease or sudden death?
Harris: The Omega-3 Index is a better predictor of sudden cardiac death than blood cholesterol is, even cholesterol fractions of LDL and HDL. It’s also better than blood triglycerides or homocysteine as a risk predictor.
 Passwater: You are making a distinction between “sudden cardiac death” and “heart disease” and even “cardiovascular disease.” Experts may view sudden cardiac death as a unique disease, but the distinction may be lost on lay people. Is my assessment fair and accurate that the Omega-3 Index is the best predictor of risk for sudden cardiac death, a very good predictor of death from cardiovascular disease, and at least as good as other popular blood tests for assessing the risk for non-fatal heart attacks?
Passwater: You are making a distinction between “sudden cardiac death” and “heart disease” and even “cardiovascular disease.” Experts may view sudden cardiac death as a unique disease, but the distinction may be lost on lay people. Is my assessment fair and accurate that the Omega-3 Index is the best predictor of risk for sudden cardiac death, a very good predictor of death from cardiovascular disease, and at least as good as other popular blood tests for assessing the risk for non-fatal heart attacks?
Harris: That’s a good summary of the state of the art.
Passwater: Is the Index a good indicator of other health problems such as cognitive function or dementia?
Harris: There are several studies suggesting that people with lower omega-3 intakes or blood levels are more likely to have cognitive dysfunction, but proof that giving omega-3 will improve the situation is lacking. We are currently studying this question in a sample of over 7,000 women who were followed for loss in cognitive function for over 10 years. We have measured their Omega-3 Index scores at the beginning of the study and will see if a higher Index was associated with a slower rate of cognitive loss.
Passwater: How about aging?
Harris: As I mentioned earlier, we did find that people who have the highest Omega-3 Index values appear to have the slowest rates of “cellular aging.” This is estimated by measuring the rate of telomere attrition, or shortening of the tips of the chromosomes. The faster the telomere section shortens, the faster the aging process (see Figure 2). In our study, those with an Omega-3 Index of about 8% “aged” at less than half the rate as those with an Index of 3%. Although not definitive, the fact that the Japanese as a population have one of the highest omega-3 index values in the world and are about the longest lived people on earth may not be a coincidence.
Passwater: Specifically, what do you measure to form your Omega-3 Index? Is the Index based on only long-chain omega-3s (EPA and DHA) or are short-chain omega-3s (ALA etc.) also included?
Harris: The Index is defined as the RBC content of EPA and DHA expressed as a percent of total RBC fatty acids. Neither ALA nor docosapentaenoic acid (DPA) are included in the Index.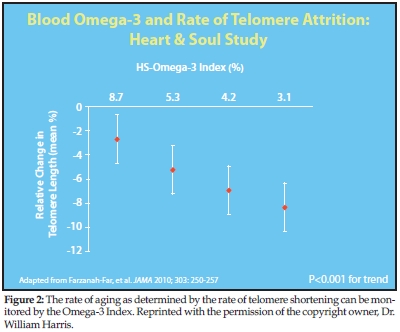
Passwater: What are good and bad “scores” with the Index and how were these determined?
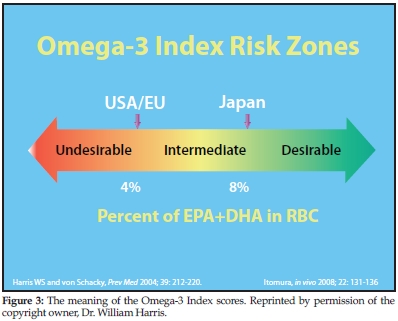
Harris: Good is >8% and bad is <4% (see Figure 3).
They were originally (2004) determined based on several studies that showed, in the aggregate, people who were at the lowest risk for death from heart disease had an average Omega-3 Index of about 8%, whereas those who were at the highest had levels of 4% or less. These numbers have been confirmed by later studies showing that people admitted for an ACS were 35% less likely to have an Omega-3 Index over 8% than normal controls, and as noted earlier, the slowest rate of cellular aging was seen at an Index >8% and the fastest at <4%.
Please keep in mind, that as with all clinical blood tests, there can be big lab-to-lab differences in measuring the Omega-3 Index due to different methods in use. The range of values will be stated for each lab by that lab on the report.
Passwater: I notice that other laboratories may also express the results in a different manner. One of the fish oil brands is even offering free tests to retailers on a limited basis.
Harris: I believe you are referring to the “omega-balance” test. Yes, the numbers that test reports are different, but the point is the same. Some places where you order the HS-Omega-3 Index test kit are: http://www.genesmart.com/pages/omega_3_index_home_blood_testing_kit/105.php
http://www.myvitalremedymd.com/order/omega-3-blood-test.php and
http://bioletics.com/content/essential-fatty-acid-status.
Passwater: How do typical Americans compare to other peoples?
Harris: The average value we’re seeing in the United States is around 4–5% whereas we’ve seen levels well over 8% in Japanese samples and over 7% in a population in Barcelona, Spain. The Koreans also seem to have quite high levels. No organized cross-country comparisons have been done to date, but this would be a great study to do as long as all the samples were analyzed by the same method.
Passwater: Do those groups with higher omega-3 levels have less heart disease?
 Harris: Typically, yes. The Japanese, Spanish, Norwegians and Koreans have coronary heart disease death rates that of 48, 92, 96 and 51 males per year per 100,000 population; in the United States, it’s 153.
Harris: Typically, yes. The Japanese, Spanish, Norwegians and Koreans have coronary heart disease death rates that of 48, 92, 96 and 51 males per year per 100,000 population; in the United States, it’s 153.
Passwater: Is this generally the rule regardless of the person’s sex?
Harris: We have not seen a significant difference in the HS-Omega-3 Index in men versus women. Now, older people tend to have higher levels than younger. This could be because they eat more fish, or possibly because of “attrition of the susceptible.” That is, people with lower levels (the susceptible) die earlier than those with higher levels, which enriches the older group with people with higher omega-3 levels.
Passwater: Is there a direct or simple correlation between the numbers obtained in the Omega-3 Index blood level and dietary intake ratio of omega-3s to omega-6s? Would an Index of 20 suggest something like a one-to-five ratio of omega-3 to omega-6 intake, or anything like that?
Harris: No. Definitely, not! Higher omega-3 levels come from higher omega-3 intakes, not lower omega-6 intakes.
Passwater: Many people today are approaching the virtual disappearance of long-chain omega-3 fatty acids in terms of the dietary ratio of omega-6 to omega-3. They point to the change in ratio over the millennia.
Harris: This is a long discussion. The omega-6:omega-3 ratio is a metric that should go away. It is too confusing and imprecise. The problems—briefly—are:
1. The ratio does not define which omega-6 and which omega-3 fatty acids are counted, so EPA and DHA are deemed to be equivalent to ALA (which is not true), and linoleic acid and arachidonic acid are considered the same (also not true).
2. There are metabolic conversions that happen in the body so that eating a certain ratio in no way translates into a certain tissue ratio.
3. You can eat deficient or excessive amounts of both omega-3 and omega-6 fatty acids and have a “healthy ratio.”
4. The ratio concept is based on the false view that omega-6 fatty acids are “bad” (usually “pro-inflammatory”) and the omega-3s are “good” (anti-inflammatory). This is far too simple and just not true; a higher omega-6 intake and blood level is associated with reduced not increased risk for CHD. So, the ratio concept is flawed from the outset and should not be promoted. Beyond that, we don’t know what Paleolithic man was eating, nor do we know what his health status was. But, of this we are sure: he did not routinely live into his 60s to 90s where modern chronic diseases become manifest, so diets that purportedly increase risk for arthritis or heart attacks would never have had their effect in someone who died of a snakebite at 16 or fell off a rock at 32.
Passwater: Agreed. The studies do show that adding EPA/DHA supplements to the diet in clinical trials do bring about the health benefits that are now becoming widely known. There are no clinical trials that I am aware of that show merely changing the ratio in the absence of increasing EPA to one gram or more brings about these results. Besides, modern diets are deeply ingrained and difficult to change. It is easier, as well as proven, that adding EPA and DHA to above one gram per day are what people should focus on.
Is there any indication that there is a harmful upper limit or does the health improvement continue to rise with the Index?
Harris: It may still be too early to answer this definitively. It only makes sense that there is a value above which there is no additional health benefit, but nobody knows what that would be. It is hard to imagine that someone at a level of 13% would be healthier than someone at 10%, but the results of the JELIS study (in Japan) and some data from Korea suggest that this may in fact be the case. We just don’t know.
Passwater: Is the Omega-3 Index test just a research technique or is it in clinical use?
Harris: Both.
Passwater: How many tests have been done in research studies?
Harris: Just our group alone has done over 20,000 tests for research projects, and about three times that amount have now been done for doctors testing their patients.
Passwater: Can physicians and patients take advantage of this test now?
Harris: Yes. Clinicians can order the test (and patients can ask their physicians to do so) through Health Diagnostic Laboratory, Inc. of Richmond, VA (www.myhdl.com). Researchers can contact OmegaQuant, LLC in Sioux Falls, SD (www.omegaquant.com) to get the test done.
Passwater: Do you now have a substantial database that can be used to learn more about real people and their everyday consumption of fats and their risk of various diseases?
Harris: Yes and no. We have a large database of clinical samples, however, we don’t know anything about other patient characteristics such as age, sex, race, other diseases, diet, supplementation status, drugs and other factors. In the Framingham Heart Study and in the Women’s Health Initiative Study, we have extensive data on health status and health outcomes that will produce several research reports in coming months to years.
Passwater: Have you done follow-up tests (before and after) with people who increase the omega-3 intake to see if the Omega-3 Index changes correspondingly?
Harris: Yes. It appears that it takes about one gram of EPA+DHA per day for about half a year to move the average person’s HS-Omega-3 Index of 4% up to the target of 8%. This will vary considerably depending on many variables, but that gives people a rough idea of where to start.
Passwater: It takes time for tissue levels to improve. Have you been able to note which forms of omega-3 yield the most improvement in the Index (on a gram per gram basis)?
Harris: This is an active area of research. Dr. von Schacky did a study comparing an ethyl ester product to a triglyceride product and found that the latter raised the Omega-3 Index to a slightly, but statistically significantly, greater extent than the former over six months. In general, ethyl esters are less well absorbed than triglycerides (especially when taken on an empty stomach). Whether krill oil (phospholipid carrier of omega-3) will be better absorbed than the triglyceride- or ethyl ester-based products remains to be seen.
Passwater: Does consuming more ALA increase EPA and DHA levels according to your experience with the Index?
Harris: No. There are some studies that showed that although ALA slightly increased the EPA portion of the Index, it ended up decreasing the DHA portion, so that the net effect on the Omega-3 Index was null. There are undoubtedly wide variations in the rate of conversion of ALA to EPA, but, on average, it’s about 4%; to DHA, <1%.
Passwater: According to your studies utilizing the Omega-3 Index, does consuming more EPA increase DHA levels?
Harris: No.
Passwater: Does consuming more DHA increase EPA levels?
Harris: Yes, but to a very small extent. A recent study found that <5% of a dose of labeled DHA appeared in shorter chain omega-3s.
Passwater: Does your test also measure trans-fats?
Harris: Yes, it does. High RBC levels of trans fats are a telling marker of a diet rich in processed oils and fats. People trying to adopt a healthier diet should see a decrease in their trans l evels.
evels.
Passwater: Are you conducting additional studies in other disease areas?
Harris: Yes, we just published a study showing differences in omega-3 status in patients with varying severities of sleep apnea, and other studies are underway in adolescent depression and cognitive decline. WF
Dr. Richard Passwater is the author of more than 40 books and 500 articles on nutrition. He is the vice president of research and development for Solgar Vitamin and Herb. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com.
Published in WholeFoods Magazine, November 2011
Appendix
Papers on the Omega-3 Index: 2004-2011
Harris WS and von Schacky C. The Omega-3 Index: A New Risk Factor for Death from CHD? Preventive Medicine 39:212-220, 2004. PMID: 15208005
Harris WS, Sands SA, Windsor SL, Ali HA, Stevens TL, Magalski A, Porter CB, Borkon AM. Omega-3 Fatty Acid Levels in Transplanted Human Hearts: Effect of Supplementation and Comparison with Erythrocytes. Circulation 110;1645-49, 2004. PMID: 15353491
Sands SA, Reid KJ, Windsor SL, Harris WS. The impact of age, body mass index, and fish intake on the EPA and DHA content of human erythrocytes. Lipids 40:343-347, 2005. PMID: 16028715
Harris WS, Gonzales M, Laney N, Sastre A, Borkon AM. Effects of Omega-3 Fatty Acids on Heart Rate in Cardiac Transplant Recipients. Am J Cardiol 98:1393-1395, 2006. PMID: 17134636
Harris WS, Reid KJ, Sands SA, Spertus JA. Blood Omega-3 and Trans Fatty Acids in Middle-Aged Acute Coronary Syndrome Patients. Am J Cardiol 99:154-158, 2007. PMID: 17223410
Harris WS, DiRienzo MA, Sands SA, George C, Astwood JD, Jones PG, Eapen AK. Stearidonic Acid Supplementation Increases Red Blood Cell and Heart Omega 3 Index in Dogs. Lipids 42:325-333, 2007. PMID: 17406927
Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis 193:1-10, 2007. PMID: 17507020
Harris WS, Pottala JV, Sands SA, and Jones PG. Comparison of the effects of fish and fish oil capsules on the n-3 fatty acid content of blood cells and plasma phospholipids. Am J Clin Nutr 86 :1621-25, 2007. PMID: 18065578
Block RC, Harris WS, Reid KJ, Sands SA, Spertus JA. EPA and DHA in blood cell membranes from acute coronary syndrome patients and controls. Atherosclerosis. 197:821-828, 2008. PMID: 17875307
Cohen BE, Garg SK, Ali S, Harris WS, Whooley MA. Red blood cell EPA and DHA concentrations are positively associated with Socioeconomic status in patients with established coronary artery disease: Data from the Heart and Soul Study. J Nutrition 138 :1135-1140, 2008. PMID: 18492846
Aarsetoey H, Pönitz V, Nilsen OB, Grundt H, Harris W, Nilsen DWT. Low levels of cellular omega-3 increases the risk of ventricular fibrillation during the acute ischaemic phase of a myocardial infarction. Resuscitation 78:258-264, 2008. PMID: 18556107
Block RC, Harris WS, Pottala JV. Determinants of blood cell omega-3 fatty acid content. The Open Biomarkers J 1:1-6, 2008. PMID: 19953197
Larson MK, Ashmore JH, Harris KA, Vogelaar JL, Pottala JV, Sprehe M, Harris WS. Effects of Omega-3 Acid Ethyl Esters and Aspirin, Alone and in Combination, on Platelet Function in Healthy Subjects. J Thromb Haemost 2008;100:634-41. (Oct). PMID: 18841286
Harris WS, Lemke SL, Hansen SN, Goldstein DA, DiRienzo MA, Su H, Nemeth MA, Taylor ML, Ahmed G, George C. Stearidonic Acid-Enriched Soybean Oil Increased the Omega-3 Index, an Emerging Cardiovascular Risk Marker. Lipids 2008;43:805-811. (Sept) PMID: 18683001
Amin AA, Menon RA, Reid KJ, Harris WS, Spertus JA Acute Coronary Syndrome Patients With Depression Have Low Blood Cell Membrane Omega-3 Fatty Acid Levels. Psychosom Med. 2008;70:856-62. (Oct). PMID: 18842751
Farzaneh-Far R, et al. Inverse association of erythrocyte n-3 fatty acid levels with inflammatory biomarkers in stable coronary artery disease: The Heart and Soul Study. Atherosclerosis 2009; 205:538-43 (Aug). PMID: 19185299.
Duda MK, O'shea KM, Tintinu A, Xu W, Khairallah RJ, Barrows BR, Chess DJ, Azimzadeh AM, Harris WS, Sharov VG, Sabbah HN, Stanley WC. Fish Oil, But Not Flaxseed Oil, Decreases Inflammation and Prevents Pressure Overload-Induced Cardiac Dysfunction. Cardiovasc Res. 2008;81:310-327. ( Nov) PMID: 19015135
Block RC, Harris WS, Reid KJ, Spertus JA. Omega-6 and trans fatty acids in blood cell membranes: a risk factor for acute coronary syndromes? Am Heart J. 2008;156:1117-23. (Dec) NIHMS75965. PMCID: PMC2596644.
Ali S, Garg SK, Cohen BE, Bhave P, Harris WS, Whooley MA. Association between omega-3 fatty acids and depressive symptoms among patients with established coronary artery disease: Data from the Heart and Soul Study. Psychother Psychosom. 2009;78:125-127 (Feb). PMID: 19223688
Shearer GC, Pottala JV, Spertus JA, Harris WS (2009) Red Blood Cell Fatty Acid Patterns and Acute Coronary Syndrome. PLoS ONE 4(5): e5444. doi:10.1371/journal.pone.0005444. PMID: 19185299
Aarsetoey H, Volker P, Grundt H, Staines H, Harris WS, Nilsen DWT. (n-3) fatty acid content of red blood cells does not predict risk of future cardiovascular events following an acute coronary syndrome. J Nutr 2009;139:1–7. PMID: 19158216
Harris WS, Thomas RM. Biological Variability of Blood Omega-3 Biomarkers. Clin Biochem 2010;43:338–340. PMID: 19733159
Carney RM, Freeland KE, Rubin EH, Rich MW, Steinmeyer BC, Harris WS. Omega-3 augmentation of sertraline in the treatment of depression in patients with coronary heart disease: a randomized controlled trial. JAMA 2009; 302:1651-1657 (October). PMID: 19843899
Shearer GS, Chen J, Chen Y, Harris WS. Myocardial infarction does not affect erythrocyte fatty acid profiles in rats. Prost Leuko Ess Fatty Acids 2009;81:411-416 (Sept). PMID: 19775878
Farzaneh-Far R, Lin J, Epel ES, Harris WS, Blackburn EH, Whooley MA. Association of marine omega-3 fatty acid levels with telomeric aging in patients with coronary heart disease. JAMA 2010;303(3):250-257. PMID: 20085953
Billman GE, Nishijima Y, Belevych AE, Terentyev D, Xu1 Y, Haizlip1 KM, Monasky1 MM, Hiranandani1 N, Harris WS, Gyorke S, Carnes CA, Janssen PML. Effects of Dietary Omega-3 Fatty Acids on Ventricular Function in Dogs with Healed Myocardial Infarctions: In Vivo and In Vitro Studies. Am J Physiol Heart Circ Physiol. Jan 22 2010 [Epub ahead of print. PMID: 20097770
Block RC, Duff R, Lawrence P, Kakinami L, Brenna JT, Shearer GC, Meednu N, Mousa S, Friedman A, Harris WS, Larson M, Georas S.The Effects of EPA, DHA, and Aspirin Ingestion on Plasma Lysophospholipids and Autotaxin. Prostagl Leukot Essent Fatty Acids. 2010 Jan 25. [Epub ahead of print] PMID: 20106646
Ebbesson SOE, Devereux RB, Cole S, Ebbesson LOE, Fabsitz RR, Haack K, Harris WS, Howard WH, Laston S, Lopez-Alvarenga JC, MacCluer JW, Okin PM, Tejero E, Voruganti VS, Wenger CR, Howard BV, Comuzzie AG. Heart Rate is Associated with Red Blood Cell Fatty Acid Concentration: the GOCADAN Study. Am Heart J, 2010;159:1020-1025. PMID: 20569715
Pottala JV, Garg S, Cohen BE, Whooley MA, Harris WS. Blood EPA and DHA Independently Predict All-Cause Mortality in Patients with Stable Coronary Heart Disease. The Heart and Soul Study. Circ:Qual Outcomes 2010;3 406-412. PMID: 20551373
Carney RM, Freedland KE, Stein PK, Steinmeyer BC, Harris WS, Rubin EH, Krone RJ, Rich MW. The Effect of Omega-3 Fatty Acids on Heart Rate Variability in Depressed Patients With Coronary Heart Disease. Psychosomat Med 2010;72(8):748-54. PMID: 20716712
Lemke SL, Vicini JL, Su H, Goldstein DA, Nemeth MA, Krul ES, Harris WS. Dietary intake of stearidonic acid enriched soybean oil increases the omega-3 index: randomized, double-blind clinical study of efficacy and safety. Am J Clin Nutr. 2010;92(4):766-75. PMID: 20739419.
Chen J, Shearer GS, Chen Q, Healy CL, Beyer AJ, Nareddy VB, Gerdes AM, Harris WS, O’Connell TD, Wang D. Omega-3 fatty acids prevent pressure overload-induced cardiac fibrosis through activation of cGMP/PKG signaling in cardiac fibroblasts. Circulation 2011;123:584-93. PMID: 21282499.
Skulas-Ray AC, Kris-Etherton PM, Harris WS, Vanden Heuvel JP, Wagner PR, West SG. Dose response effects of omega-3 fatty acids on triglycerides, inflammation, and endothelial function in healthy people with moderate hypertriglyceridemia. Am J Clin Nutr. 2011;93:243-52. PMID:21159789.
Aarsetøy H, Aarsetøy R, Lindner T, Staines H, Harris WS, Nilsen DWT. Low Levels of the Omega-3 Index are Associated with Sudden Cardiac Arrest and Remain Stable in Survivors in the Subacute Phase. Lipids 2011;46:151-61. PMID:21234696
Moyers B, Farzaneh-Far R, Harris WS, Garg S, Na B, Whooley MA. Relation of Whole Blood n-3 Fatty Acid Levels to Exercise Parameters in Patients With Stable Coronary Artery Disease (from the Heart and Soul Study). Am J Cardiol. 2011;107:1149-54. PMID:21306696
Sala-Vila A, Harris WS, Cofán M, Pérez-Heras AM, Pintó X, Lamuela-Raventós RM, Covas M-I, Estruch R, Ros E. Determinants of the omega-3 index in a Mediterranean population at increased risk for coronary heart disease. Brit J Nutr 2011; epub before print March 30. PMID:21450116
Billman GE, Harris WS. Effect of Dietary Omega-3 Fatty Acids on the Heart Rate and the Heart Rate Variability Response to Myocardial Ischemia or Submaximal Exercise. Am J Physiol Heart Circ Physiol. 2011 Apr 1. [Epub ahead of print]. PMID:21460198
Salisbury AC, Amin AP, Harris WS, Chan PS, Gosch KL, Rich MW, O'Keefe JH Jr, Spertus JA. Predictors of omega-3 index in patients with acute myocardial infarction. Mayo Clin Proc. 2011 Jul;86(7):626-32.
Ladesich JB, Pottala JV, Romaker A, Harris WS. Membrane Level of Omega-3 Docosahexaenoic Acid Is Associated with Severity of Obstructive Sleep Apnea. J Clin Sleep Med 2011; 7:391-396.
von Schacky C and Harris WS. Cardiovascular benefits of omega-3 fatty acids. Cardiovasc Res 73:310-315, 2007. PMID: 16979604
Harris WS. Omega-3 Fatty Acids and Cardiovascular Disease: A Case for Omega-3 Index as a New Risk Factor. Pharma Res 55:217-273, 2007.
Von Schacky C, Harris WS. Cardiovascular risk and the omega-3 index. J Cardiovasc Med 8:S46-S49, 2007. PMID: 17876200
Harris WS, Von Schacky C. Omega-3 fatty acids, acute coronary syndromes and sudden cardiac death. Curr Cardiovasc Risk Rpt 2008;2:161-166.
Harris WS. The omega-3 index as a risk factor for coronary heart disease. Am J Clin Nutr 2008;87(suppl):1997S-2002S.
Harris WS. The Omega-3 Index: From biomarker to risk marker to risk factor. Curr Athero Rept 2009;11:411-417. Nov; PMID: 19852881
Harris WS. Blood omega-3 levels predict the rate of cellular aging. Lipid Spin (NLA publication) Spring, 2010.
Harris WS. The Omega-3 Index: Clinical Utility for Therapeutic Intervention. Curr Cardiol Rep. 2010 (Sept). 12:503–508. PubMed PMID: 20809235.
Harris WS, Klurfeld DM. Twentieth-century trends in essential fatty acid intakes and the predicted omega-3 index: evidence versus estimates. Am J Clin Nutr. 2011 (Mar);93:907-908. PMID: 21430117










