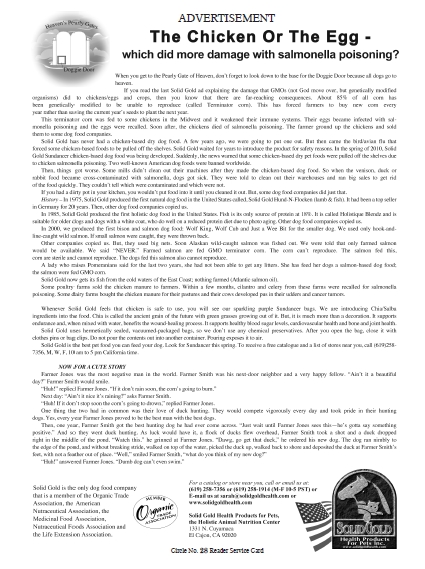
Let’s clarify what a recent study of multivitamins actually found and put this one study in perspective with the larger body of scientific evidence on multivitamins. The “take home” message is that most people are not getting the recommended amounts of vitamins and minerals solely from their diets and are healthier with supplementation to overcome their multiple deficiencies. Secondly, no, there is no valid scientific evidence that taking multivitamins shortens anyone’s life. Dr. Robert Smith and I will discuss some of the most important details later in this column.
It is absolutely amazing as to what nonsense can be passed off as science these days! Almost just as amazing is how little scrutiny today’s reporters give articles published in some of the medical journals that are so dependent on pharmaceutical advertising. One month, coffee is reported to be good for you and the next mont h, it is found to be a killer. The same goes with aspirin or alcohol. No wonder the public is confused.
h, it is found to be a killer. The same goes with aspirin or alcohol. No wonder the public is confused.
Today, journals depend on massive self-serving press releases to vie for media attention. At one time, scientists merely let their work “speak” for itself after close inspection by other scientists. They did not gather in front of the TV cameras and shout “Look at me!” They let their research do all the talking.
Is it 1970 all over again? In the 1970s, the only information about nutrition that made national news was negative news reported by “reporters” who did not understand the scientific methodology or who were not scientifically trained and who reported every new study in isolation as if it were the only study on the subject ever conducted.
The concept of total body of scientific evidence was lost on these sensationalistic “reporters.” Even if they were interested in checking the body of scientific literature for other studies, it would have been difficult because in the 1970s, there was no Internet or PubMed electronic database kept by the National Library of Medicine. Unfortunately, even if reporters check PubMed (Medline) today, they still won’t find many positive studies because several complementary or integrative medicine journals, such as the Journal of Orthomolecular Medicine, are not included in the PubMed database.
These “reporters’” motive was evidently to get their face on national TV or their byline as a headline in the press without regard for the consequences of reporting inaccurate and misleading out-of-scientific-context information. This tactic would lead to their personal advancement without much concern for the result of their misinformation on the public. These “reporters” felt little responsibility for the whole truth—only “accuracy” in reporting the study no matter how flawed it was. The more startling fear they could put on the faces of their anchors, the better their chances of being given another assignment.
misinformation on the public. These “reporters” felt little responsibility for the whole truth—only “accuracy” in reporting the study no matter how flawed it was. The more startling fear they could put on the faces of their anchors, the better their chances of being given another assignment.
In the 1970s, reporting on vitamins often fell into the duties of food editors. They knew their recipes and food sales, but they were not scientists. Through the ensuing decades, specialty fields evolved and science matters were covered by science writers and medical matters were covered by medical writers, and the coverage of vitamin research greatly improved. Now, there seems to be a cut-back in staffing of many media outlets and as a consequence, reporting on medical and nutrition matters is suffering.
The sensationalistic coverage of a recent so-called study of multivitamins is an example. By the time the scientific community can respond and put this study in proper scientific perspective, the damage will already have been done as countless people needlessly give up their multivitamin supplements because of an unfounded fear of dying prematurely. Most people need these multivitamins to supplement their vitamin-deficient diets, but now many will incorrectly think that they may shorten their lifespan.
Fortunately, at least one scientist took the time and energy to respond to the situation. I was pleased to find a news release from the Orthomolecular News Service (OMNS) in my inbox. OMNS is one of my very favorite organizations. The outstanding press release was written by Robert G. Smith, Ph.D., of the University of Pennsylvania.
I knew that you would also be interested in what Dr. Smith wrote, so I called upon him to chat with us about this recent publication concerning multivitamins.
Dr. Smith is a research associate professor at the University of Pennsylvania, Department of Neuroscience. He is a member of the Institute for Neurological Sciences and the author of several dozen scientific papers and reviews.
 Dr. Smith is a scientist who studies the neural circuitry of the eye and brain. He received his Ph.D. at the University of Pennsylvania, and then continued his education with a postdoctoral fellowship at the university. He has studied the circuitry of the retina as a research-track scientist at the university for the last two decades. Dr. Smith studies how neural circuits function, and which signal processing functions they perform to allow us to see color, motion, contrast and at night. He is an expert in neurophysiological properties of neurons, and constructing biophysically based computer models of neural circuits. He is an avid photographer of portraits and natural landscapes.
Dr. Smith is a scientist who studies the neural circuitry of the eye and brain. He received his Ph.D. at the University of Pennsylvania, and then continued his education with a postdoctoral fellowship at the university. He has studied the circuitry of the retina as a research-track scientist at the university for the last two decades. Dr. Smith studies how neural circuits function, and which signal processing functions they perform to allow us to see color, motion, contrast and at night. He is an expert in neurophysiological properties of neurons, and constructing biophysically based computer models of neural circuits. He is an avid photographer of portraits and natural landscapes.
Passwater: Dr. Smith, thank you for your rapid critique of the recent multivitamin study. Your responsible action will help many, many people. What brought your research interests to nutrition and neuroscience in the first place?
Smith: As a child, I learned about nature from my grade school nature teacher, who took the class on field trips, teaching us about plants and animals in a local forest. This gave me an avid interest in the environment and in health, and in how animals see and sense the environment. We discussed how birds can navigate on a long migration, but the research had not yet been performed that established their ability to sense magnetic fields. As a young adult, I learned about nutrition by reading, Let’s Eat Right to Keep Fit, by Adelle Davis (1). I also read Silent Spring by Rachel Carson (2), learning about the importance of keeping the environment clean so that we can have a healthy world to live in and healthy food to eat. I first became interested in orthomolecular medicine in 1970 when I read Linus Pauling’s book, Vitamin C and the Common Cold (3). This book explained that taking an adequate dose of vitamin C can prevent colds and hasten recovery from them. Although it was controversial, I was fascinated, and have continued taking a daily vitamin C supplement. Soon after, I went on to read, Diet for a Small Planet, by Frances Moore Lappé (4), which popularized nutrition by explaining how to eat efficiently and sustainably.
From my childhood interest in nature, I had always been interested in how we see and sense the world. In my teens, I constructed short-wave radios, and became interested in electronics. In my 20s, I taught myself analog and digital electronics by building electronic devices such as a digital multimeter and an electrocardiographic amplifier. I designed and built a home-brewed micro-computer, became active in the local hobby computer society, and progressed into computer hardware and software. I got a job at the University of Pennsylvania as a computer engineer, designing data-acquisition boards and software to run them for the neuroscientists at Penn.
world. In my teens, I constructed short-wave radios, and became interested in electronics. In my 20s, I taught myself analog and digital electronics by building electronic devices such as a digital multimeter and an electrocardiographic amplifier. I designed and built a home-brewed micro-computer, became active in the local hobby computer society, and progressed into computer hardware and software. I got a job at the University of Pennsylvania as a computer engineer, designing data-acquisition boards and software to run them for the neuroscientists at Penn.
In my early 30s, I enrolled in the graduate program at Penn, studying the retinal circuits that allow us to see. I utilized my computational skills to develop a computer language called “Neuron-C,” which allows one to construct a model of a neural circuit and perform an electrophysiology experiment on it. This allows the researcher to explore properties of the circuit that could not be done on live tissue. I continue to use this tool to study the functional properties of the retina. In this research, I became knowledgeable about eye diseases and the physiological requirements of neural tissue, including vitamins such as B-vitamins and vitamins C and E, and essential nutrients such as magnesium and zinc.
Over the last five years, I developed an avid interest in learning about the vitamins and nutrients that are essential for the body. Searching on PubMed, I found many scientific papers about research on vitamins that appeared to contradict commonly held beliefs about nutrition and supplements. I read, Vitamin C: The Real Story, The Remarkable and Controversial Healing Factor, by Hickey and Saul (5), and found that nutrition science has progressed rapidly from the 1970s, and has largely vindicated the ideas in Pauling’s book. I read several books on vitamin D, learning that most people in North America are deficient. I started taking vitamin D supplements, finally increasing my daily dose to 10,000 IU to achieve an adequate blood level. I resolved to spread the word about these and other important vitamins and nutrients. I’ve tried to learn more about our need for vitamins and nutrients by reading many books and recent research papers on the beneficial effects of vitamins and nutrients on our health.
Passwater: As I mentioned in this column two months ago, a study by Dr. Jeff Blumberg in 1997 reported that “improving nutritional practices could potentially delay the onset of cardiovascular disease, stroke and osteoporosis by five years, thus saving $89 billion in health 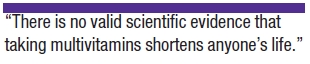 care costs annually” (6). Another example is the Lewin Study, which reported that spending just pennies a day on supplements per person can reduce our national healthcare expenditures by $24 billion over five years (7). Both studies were published before it was determined that higher levels of vitamin D could provide an even larger cost reduction. Such impact on our national health care costs is not surprising, since about 92% of Americans do not receive the RDI for one or more nutrients. Another study in the European Journal of Nutrition shows that antioxidant nutrient supplementation reduced cancer mortality by 48% and all-cause mortality was reduced by 42% over the 11 years of study (8). Still another study shows that multivitamins help keep cells younger (and thus healthier) by improving telomere length (9).
care costs annually” (6). Another example is the Lewin Study, which reported that spending just pennies a day on supplements per person can reduce our national healthcare expenditures by $24 billion over five years (7). Both studies were published before it was determined that higher levels of vitamin D could provide an even larger cost reduction. Such impact on our national health care costs is not surprising, since about 92% of Americans do not receive the RDI for one or more nutrients. Another study in the European Journal of Nutrition shows that antioxidant nutrient supplementation reduced cancer mortality by 48% and all-cause mortality was reduced by 42% over the 11 years of study (8). Still another study shows that multivitamins help keep cells younger (and thus healthier) by improving telomere length (9).
Multivitamins are intended to fill the gaps between overt deficiencies and the recommended dietary intakes in an effort to have at least average health. Multivitamins are not intended to provide optimal nourishment. Additional supplementation is needed for optimal nourishment to reduce the risk of diseases. One milligram of aspirin is not likely to cure a bad headache, whereas 300 milligrams may. It would be unfair to say that aspirin does not cure headaches based on a study using only one milligram.
In spite of the many peer-reviewed studies showing that nutrients improve health, reduce disease and improve mortality, one recently released study incorrectly suggests that multivitamin and nutrient supplements can increase the mortality rate in older women (10). What are your concerns about the study’s methods and significance?
Smith: The study was observational, in which participants filled out a survey about their eating habits and their use of supplements. Although this type of study is widespread and can be very important in discovering the benefit of a specific diet, and can give clues about the cause of a medical condition, it cannot determine cause and effect. The study reports only a small increase in overall mortality (1%) from those taking multivitamins. This is not much larger than would be expected by chance. Generalizing from such a small effect is not scientific.
Passwater: Please help us understand the numbers reported in this study. There is always a question of their mathematical statistical “significance” and real-world significance in meaning. Would you please explain how “significant” they are?
Smith: The realm of statistics can sometimes be very confusing for non-statisticians. The p-values and confidence intervals in the Mursu et al. (2011) paper, from groups of several hundred to several thousand vitamin users, reflect the probability that the result is different than chance. If the result is closer to w hat is expected by chance, the p-value is higher. A standard value for p-values to assure significance is <0.05. But, of course, that doesn’t really say much that can help, because it only means that, assuming a standard or “normal” distribution, the likelihood that the result is due to random fluctuations is less than 5%. Likewise, the confidence intervals give a range of values for the “hazard ratio” (the relative risk) within which the actual parameter is likely to fall. The confidence interval used is 95%, which means that, given the sampling error, and assuming a normal distribution, there is a 5% likelihood that the hazard ratio is outside that range. These numbers, therefore, contain assumptions and don’t tell us very securely how much random fluctuation might be involved. A higher p-value means there is more uncertainty because, for example, the number of people is too small or there were unknown factors that influenced the result. In that case, the difference actually observed is more likely to have been due to chance. If the risk numbers are near to what is expected from chance, that is, they don’t reflect an obvious result, then statistics won’t help—for many people they simply add to the confusion.
hat is expected by chance, the p-value is higher. A standard value for p-values to assure significance is <0.05. But, of course, that doesn’t really say much that can help, because it only means that, assuming a standard or “normal” distribution, the likelihood that the result is due to random fluctuations is less than 5%. Likewise, the confidence intervals give a range of values for the “hazard ratio” (the relative risk) within which the actual parameter is likely to fall. The confidence interval used is 95%, which means that, given the sampling error, and assuming a normal distribution, there is a 5% likelihood that the hazard ratio is outside that range. These numbers, therefore, contain assumptions and don’t tell us very securely how much random fluctuation might be involved. A higher p-value means there is more uncertainty because, for example, the number of people is too small or there were unknown factors that influenced the result. In that case, the difference actually observed is more likely to have been due to chance. If the risk numbers are near to what is expected from chance, that is, they don’t reflect an obvious result, then statistics won’t help—for many people they simply add to the confusion.
Note that there are several versions of the risk numbers, for different assumptions about correcting the risks using multivariate analysis. They are recalculations and are farther removed from the raw data. They are in many cases quite different, which for many readers may add to the confusion. In this study, the absolute difference in risk for multivitamins was ~1%, but the risk after recalculation was quoted as 2.4%. The problem is, that 1% is a small difference, small enough that it could readily originate in a combination of other effects, such as random fluctuation or bias from the “doctor advice” or “proactive education” effects described below. The recalculation is an attempt to remove extraneous effects, but cannot entirely remove them or the random component. For some perspective on this, the random fluctuation expected in a group of 10,000 people who have a particular condition is 1%, more or less. A group of ~5,000 (such as the one for multivitamin use) would be expected to have a higher random fluctuation.
Passwater: The data were “adjusted” in two different attempts. To me, the “re-adjustment” appears to be an effort to find a fudge factor to confound the data. As just one example, the “adjustment” for eating fruits and vegetables appears to be just that—an attempt to dilute the positive effects of multivitamins by penalizing those who ate more fruits and vegetables and also took multivitamins. Instead of reporting what was actually found, the data are altered to “adjust” any deaths occurring earlier than expected in a group of people eating more fruits and vegetables on their taking of multivitamins—even for accidental deaths.
I wonder how many of the reporters understand the limitations of the numbers and the study’s conclusions. As you said, it is an “observational” study.
Not all “studies” are of equal scientific value. Unlike Shakespeare’s observation about a rose by any other name would smell as sweet, some so-called health studies may not be so scientific!
In the hierarchy of scientific studies, how do observational studies compare with other studies such as case-controlled and placebo-controlled, double-blind, randomized trials?
Smith: An observational study does not give any treatment to the participants, but merely records in a group of people how many who have a certain diet or lifestyle get a specific medical condition such as heart disease. A longitudinal study tests different treatments over time on the same people. A cross-sectional study examines many people at a particular time. A prospective study looks forward in time, taking a group of similar people who differ in their lifestyle or diet and tabulating how the differences affect their likelihood of getting a specific condition. A retrospective study looks backward in time, taking a group of people with a specific condition and, for example, tabulating how many of them had a specific diet or lifestyle. When such studies are case-controlled, they compare two or more groups that differ in the original condition (e.g., some who have heart disease and some who do not) and then tabulate how these groups differed in their lifestyle or diet.
Passwater: So, this is not a study where supplements or a placebo (inert-pill) were given over time and the participants followed closely and monitored to ensure that the pills were taken and absorbed.
Smith: Yes, that is correct. The study did not administer any treatment or placebo to the participants. Further, it was 18 years long and depended on their recall of what diet and supplements they took. This leaves open the possibility, occurring in many of us throughout our lives, that memory over many years is not always accurate.
Passwater: It is not even a study using a single formula or type of pill, but a grouping of various pills of various ingredients and dosages.
Smith: Yes, many of the participants took a multivitamin, but some took other specific supplements. The study actually reported that taking supplements of B-complex, vitamins C, D, E, and calcium and magnesium were associated with a lower risk of mortality. But, this was not emphasized in the abstract, leading the non-specialist to think that all supplements were associated with mortality. The report did not determine the amounts of vitamin and nutrient supplements taken, nor whether they were artificial or natural. Further, most of the association with mortality came from the use of iron and copper supplements, which are known to be potentially inflammatory and toxic when taken by older people, because they tend to accumulate in the body (11–13). The risk from taking iron supplements should not be generalized to imply that all vitamin and nutrient supplements are harmful.
Also, the known safety of vitamin and nutrient supplements when taken at appropriate doses was not taken into account. The participants most likely took only a multivitamin tablet, which contains low doses. Much higher doses of most vitamins are also safe (13, 14), implying that the low doses in common multivitamin tablets are very safe. Further, because each individual requires different amounts of vitamins and nutrients, some people must take much higher doses for best health (15, 16).
Passwater: It is a good point that the positive associations were mentioned in the full report, but not in the abstract, which is all that most reporters read. Vitamin B complex was associated with a 7% reduction in mortality, vitamin C was associated with a 4% reduction in mortality, vitamin D was associated with an 8% reduction in mortality, magnesium was associated with a 3% reduction in mortality, selenium was associated with a 3% reduction in mortality and zinc was associated with a 3% reduction in mortality. The numbers for vitamin D are interesting. The raw data show an 8% reduction in mortality even at the low multivitamin level dosage, whereas the study authors comment, “We found no evidence of benefit for vitamin D.”
I certainly agree with you about there being at least a plausibility concerning the copper numbers. This should be investigated more closely. Settings statistics aside, I personally can’t be convinced of anything based on 24 deaths in a 38,000-person study over 18 years. Yes, the number of women (529) in the “copper usage” group is also small and the stats show the proportion is higher than desired, but we need to look at more numbers in the observed group.
How reliable and accurate are dietary recall questionnaires mailed to the participants? Do they represent what a person may have taken over several years or only what they recall recently?
Smith: The study lacks scientific plausibility for several reasons. It tabulated results from surveys of 38,000 older women, based on their recall of what they ate over an 18-year period. But they were only surveyed 3 times during that period, relying only on their memory of what foods and supplements they took. This factor alone causes the study to be unreliable.
Passwater: What are some of the other flaws with this study?
Smith: Some of these women smoked (~15%) or were previously smokers (~35%), some drank alcohol (~45%), some had high blood pressure (~40%), and many of them developed heart disease and/or cancer. Some preexisting medical conditions were taken into account by adjusting the risk factors, but this caused the study to contradict what we already know about efficacy of supplements. For example, the study reports an increase in mortality from taking vitamin D, when adjusted for several health-relevant factors. However, vitamin D has recently been clearly shown to be helpful in preventing heart disease (16) and many types of cancer (17), which are major causes of death. Furthermore, supplement users were twice as likely to be on hormone-replacement therapy, which is a more plausible explanation for increased mortality than taking supplements.
Also, the effect of doctor recommendations was not taken into account. By their own repeated admissions, medical doctors and hospital nutritionists are more likely to recommend a daily multivitamin, and only a multivitamin, for their sicker patients. The study did not take this into account. All it did was tabulate deaths and attempt to correct the numbers for some prior health conditions. The numbers reported do not reflect other factors such as developing disease, side effects of pharmaceutical prescriptions or other possible causes for the mortality. The study only reports statistical correlations, and gives no plausible cause for a claimed increase in mortality from multivitamin supplements.
In addition, the effect of education was not taken into account. When a doctor gives advice about illnesses, well-educated people will often respond by trying to be proactive. Some will take drugs prescribed by the doctor, and some will try to eat a better diet, including supplements of vitamins and nutrients. This is suggested by the study itself: the supplement users in the survey had more education than those who did not take supplements. It seems likely, therefore, the participants who got sick were more likely to have taken supplements. Because those who got sick are also more likely to die, it stands to reason that they would also be more likely to have taken supplements. This effect is purely statistical; it does not represent an increase in risk that taking supplements of vitamins and essential nutrients will cause disease or death. This type of statistical correlation is very common in observational health studies and those who are health-conscious should not be confounded by it.
Passwater: How would you summarize this study?
Smith: In an observational study of older women in good health, it was said that those who died were more likely to have taken multivitamin and nutrient supplements than those who did not. The effect was small, and does not indicate any reason for disease or death. Instead, the study’s methods suggest that people who have serious health conditions take vitamin and mineral supplements because they know that supplements can help. Indeed, the study showed a benefit from taking B-complex, C, D, and E vitamins, and calcium and magnesium. Therefore, if those wanting better health would take appropriate doses of supplements regularly, they would likely continue to achieve better health and longer life.
Passwater: You are on the editorial board for the OMNS and have written some of the OMNS releases. Can our readers subscribe to this free service or is it only for the media?
Smith: The OMNS releases are in the style of a press release for the media, but anyone can sign up to receive it on the OMNS Web site.
Passwater: Where can our readers find more information about Orthomolecular Medicine?
Smith: A great website is http://orthomolecular.org, which contains many links and references. The OMNS press releases are available at:  http://orthomolecular.org/resources/omns.
http://orthomolecular.org/resources/omns.
Passwater: I, and our readers, thank you for clarifying the science involved with this sensationalistic article on multivitamin supplements. The readers can decide for themselves which has the greatest risk and benefit. All they have to ask is which is the greater risk if the report is wrong and which report is more likely to be right in the light of all that is known about the subject. WF
Dr. Richard Passwater is the author of more than 40 books and 500 articles on nutrition. He is the vice president of research and development for Solgar, Inc. Dr. Passwater has been WholeFoods Magazine’s science editor and author of this column since 1984. More information is available on his Web site, www.drpasswater.com.
References
1. A. Davis, Let’s Eat Right to Keep Fit (Harcourt Brace and Company, New York, NY, 2008).
2. R. Carson, Silent Spring (Houghton Mifflin, New York, NY, 1962, Mariner Books, 2002).
3. L. Pauling, Vitamin C and the Common Cold (W.H. Freeman and Co., San Francisco, CA, 1970, 1976).
4. F.M. Lappé, Diet for a Small Planet (Ballantine Books, New York, NY, 1971, 1991).
5. S. Hickey and S.W. Saul, Vitamin C: The Real Story, the Remarkable and Controversial Healing Factor (Basic Health Publications, Laguna Beach, CA, 2008).
6. J. Blumberg, “Public Health Implications of Preventive Nutrition,” in A. Bendich and R.J. Decklebaum, Eds., Preventive Nutrition (Humana Press, Totowa, NJ, 1997).
7. The Lewin Group “An Evidence-Based Study of the Role of Dietary Supplements in Helping Seniors Maintain Their Independence,” prepared for The Dietary Supplement Education Alliance (2006).
8. K. Li, et al., “Vitamin/Mineral Supplementation and Cancer, Cardiovascular, and All-Cause Mortality in a German Prospective Cohort (EPIC-Heidelberg),” Eur. J. Nutr. Published online ahead of print July 22, 2011, doi: 10.1007/s00394-011-0224-1.
9. Q. Xu, et al., “Multivitamin Use and Telomere Length in Women,” Am. J. Clin. Nutr. 89 (6) 1857–1863 (2009).
10. J. Mursu, et al., “Dietary Supplements and Mortality Rate in Older Women. The Iowa Women’s Health Study,” Arch. Intern Med. 171(18), 1625–1633 (2011).
11. T.F. Emery, Iron and your Health: Facts and Fallacies (CRC Press, Boca Raton, FL, 1991).
12. V.F. Fairbanks, “Iron in Medicine and Nutrition,” in M.E. Shils, et al., Eds. Modern Nutrition in Health and Disease, 9th Ed. (Williams & Wilkins, Baltimore, MD, 1999).
13. A. Hoffer and A.W. Saul. Orthomolecular Medicine for Everyone: Megavitamin Therapeutics for Families and Physicians (Basic Health Publications, Laguna Beach, CA, 2008).
14. S.J. Padayatty et al., “Vitamin C: Intravenous Use by Complementary and Alternative Medicine Practitioners and Adverse Effects,” PLoS One. 5 (7), e11414 (2010).
15. R.J. Williams and G. Deason, “Individuality in Vitamin C Needs,” Proc. Nat. Acad. Sci. USA 57, 1638–1641 (1967).
16. J. Parker et al., “Levels of Vitamin D and Cardiometabolic Disorders: Systematic Review and Meta-Analysis,” Maturitas. 65 (3), 225–236 (2010).
17. J.M. Lappe et al., “Vitamin D and Calcium Supplementation Reduces Cancer Risk: Results of a Randomized Trial,” Am. J. Clin. Nutr. 85 (6), 1586–1591 (2007).
Note
Also of Interest: Orthomolecular Medicine News Service, April 29, 2010. Multivitamins Dangerous? Latest News from the World Headquarters Of Pharmaceutical Politicians, Educators and Reporters. http://orthomolecular.org/resources/omns/v06n15.shtml
Published in WholeFoods Magazine, December 2011










